01 October 2022 | Healthcare
Healthcare Q3 ’22 Recap
By workweek
Three quarters down, one to go. In this article, I’ll wrap up the content I published in Q3. Consider this your Q3 Recap Guide.
If you still don’t know what happened in Q1 and Q2, don’t fret. Catch up below:
INSURANCE
The Three Dooming Insurance Cliffs
Americans will face three health insurance cliffs within the next half-decade, resulting in millions of uninsured individuals and families. Here are the three types of insurance programs at risk:
Medicaid/CHIP: The Family First Coronavirus Response Act (2020) increased states’ Medicaid funding by 6.2% for them to provide continuous insurance enrollment for Medicaid enrollees. So, even if an individual’s income exceeded the upper limit to qualify for Medicaid, they’d maintain insurance coverage. Medicaid/CHIP enrollment consequently increased 25% compared to pre-pandemic numbers, providing 17 million eligible adults and children with insurance coverage.
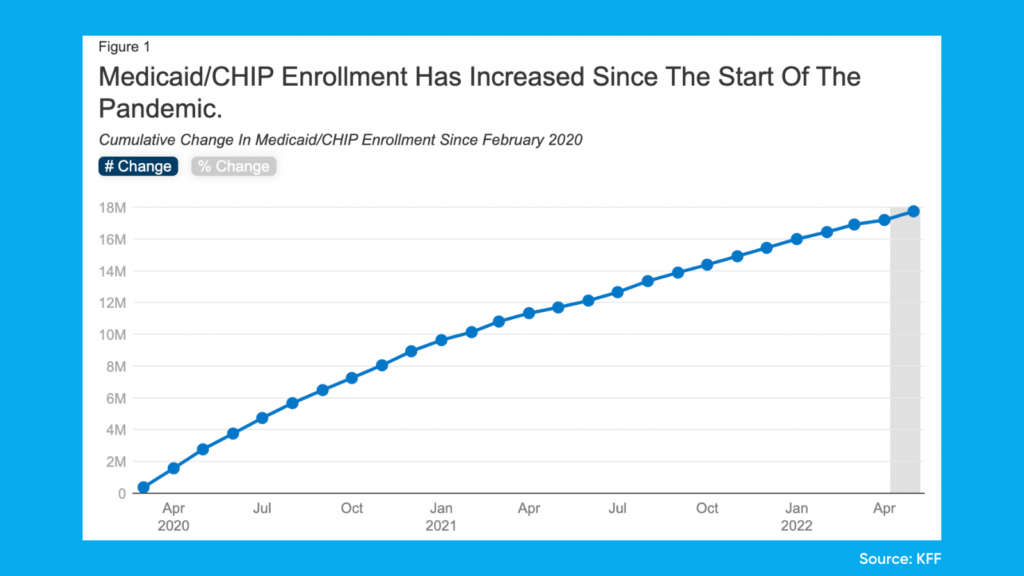
Continuous enrollment will end as soon as the public health emergency ends, resulting in 5.3 million to 14 million Americans losing insurance coverage. The Biden administration is preempting the efflux of Medicaid enrollees by investing $100 million in ACA Marketplace navigators. Navigators are organizations trained to help consumers, small businesses and their employees navigate insurance options through the ACA marketplace. Part of this funding will go to navigators to help eligible Medicaid beneficiaries transition to ACA marketplace plans.
Affordable Care Act Marketplace Insurance: The American Rescue Plan Act (2021) expanded access to the Affordable Care Act’s insurance marketplace by enhancing tax credits, essentially eliminating the subsidy cliff. This means if you make more than 400% of the federal poverty level, you won’t pay more than 8.5% of your income in premiums. Consequently, 14.5 million Americans signed up for ACA marketplace health insurance during open enrollment this year, a 21% increase from 2021.
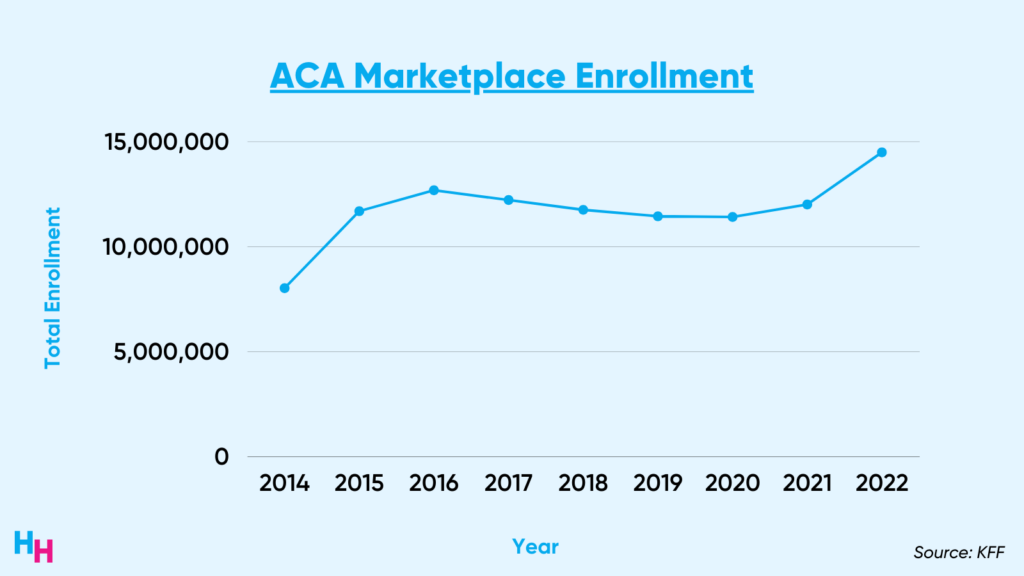
Funding for the ACA’s enhanced tax credits was set to expire by the end of the year, but the Inflation Reduction Act added $64 billion in funding to extend the enhanced tax credits. However, the funding will expire in three years, likely resulting in hundreds of thousands of Americans losing insurance due to unaffordability.
Postpartum Medicaid: The American Rescue Plan Act (ARPA) also allows states to extend postpartum Medicaid coverage from 60 days after delivery to 12 months. Thirty-four states have implemented or plan to implement the extension with full Medicaid benefits. Recall that federal law requires states to provide pregnancy-related Medicaid coverage for up to 60 days postpartum. This coverage, however, provides pregnancy-related Medicaid benefits—not full Medicaid benefits. The ARPA postpartum Medicaid coverage extension began in April of this year and will expire in 5 years. Because of Medicaid’s continuous enrollment, pregnant women already maintained insurance coverage after 60 days postpartum. Therefore, it’s unclear how many pregnant women will be at risk of Medicaid disenrollment after the funding to extend Medicaid coverage expires, but I assume it will be significant.
Dive Deeper:
DRUG PRICING
Cheap Medications—Wishful Thinking?
Will prescription medications such as insulin ever be affordable for all Americans? Maybe.
One of the key areas in the $433 billion Inflation Reduction Act of 2022 focused on lowering out-of-pocket medication spending. These measures include:
- $2,000/year out-of-pocket cap on drug costs for Medicare beneficiaries. Currently, no limit exists, forcing many to pay $10,000+ dollars per year.
- Direct negotiations between Medicare and pharma companies over certain high-cost drugs.
- Inflation rebates, requiring drug companies to refund Medicare beneficiaries and private insurance for increases in drug prices that exceed the inflation rate.
- Free vaccines for Medicare beneficiaries.
While the legislation will greatly benefit patients, reducing out-of-pocket medication spending, House Republicans want to repeal the latest drug pricing reform. They argue that by allowing direct negotiations between Medicare and pharma companies over certain high-cost drugs, pharmaceutical companies will reap less revenue, stifling drug innovation. This is the classic argument for not wanting the federal government to negotiate drug prices. Since the argument has “some” merit, two healthcare experts proposed a $20 billion biomedical innovation fund to offset drug pricing negotiations by incentivizing innovation. Such a fund may work, given Operation Warp Speed incentives helped produce Pfizer’s vaccine within months of the pandemic. Will the government ever create such a fund? TBD.
Cali Insulin
One hot topic left out of the Inflation Reduction Act was unaffordable insulin prices for 7 million Americans. California took the matter into its own hands by announcing the state would manufacture its own insulin to make the medication more affordable for Californians with insulin-dependent diabetes.
California will allocate $100M of its state budget to lower insulin costs:
- $50 million to build the insulin manufacturing plant.
- $50 million to cover the costs of manufacturing and distributing insulin.
While it’s unclear what insulin will be priced at for Californians, it’s assumed it’ll be “low-cost.”
Solutions thus far to address high insulin prices have been Band-Aid solutions. Colorado, for example, has set a $100/month limit on what Coloradans pay for insulin while the federal government is trying to cap insulin at $35/month. California, however, is directly addressing the root cause of the high insulin price problem: the drug supply chain.
Dive Deeper:
- California to Produce its Own Insulin
- How the Inflation Reduction Act Will Lower Out-of-Pocket Drug Spending
PUBLIC HEALTH
Global Warming and Contaminated Water
From unprecedented heat waves in Europe to a water crisis in Jackson, Mississippi, Q3 was no short of urgent public health issues.
Heat Waves
Western Europe experienced an unprecedented heat wave back in July. Fires ensued, high ozone levels exacerbated respiratory illnesses and airport runways melted. Given Western European countries infrequently experience such heat waves, they were unprepared for such temperatures—only three to five percent of Britons have air conditioning, for example.
Big picture: human-induced climate change is a world crisis. And, we humans—specifically those in industrialized countries—are largely to blame, given our reliance on fossil fuels that increase the concentration of greenhouse emissions. Ironically, U.S. hospitals are the world’s thirteenth largest emitters of greenhouse gasses, contributing 10% to global emissions (higher than the entire UK).
As I said in my article, there are a plethora of interventions to combat climate change. It’s just about getting everyone on board now—not later.
Don’t Drink the Water
Thousands of Jackson, Mississippi, residents were without water following water plant failures back in late August. No water to shower. No water to flush the toilet. No water to drink. For years, the city has grappled with its broken water system and subsequent public health consequences. The city simply doesn’t have enough tax revenue or state funds to update its water plants. The problem stems from white flight, where white residents have fled the city, draining financial resources.
Water plants in advanced nations shouldn’t be so vulnerable that a bout of bad weather wreaks havoc on the system, as exampled in Jackson. Access to clean water is essential for public health. Nearly 25% of the world population lacks access to clean water—who would have thought that included residents of the U.S.?
Dive Deeper:
BUSINESS
Amazon Acquires One Medical for $3.9 Billion
Amazon announced it would acquire hybrid primary care company One Medical for $3.9 billion, marking one of Amazon’s largest acquisitions to date. Amazon is creating a fully integrated healthcare platform. Their healthcare products and services include fitness wearables, caregiver services, pharmacy, patient care and groceries. Now, they’re deepening their patient care vertical. Amazon has the potential to transform the consumer—the patient—experience by streamlining its logistics, consumer data, technology and omnipresent footprint.
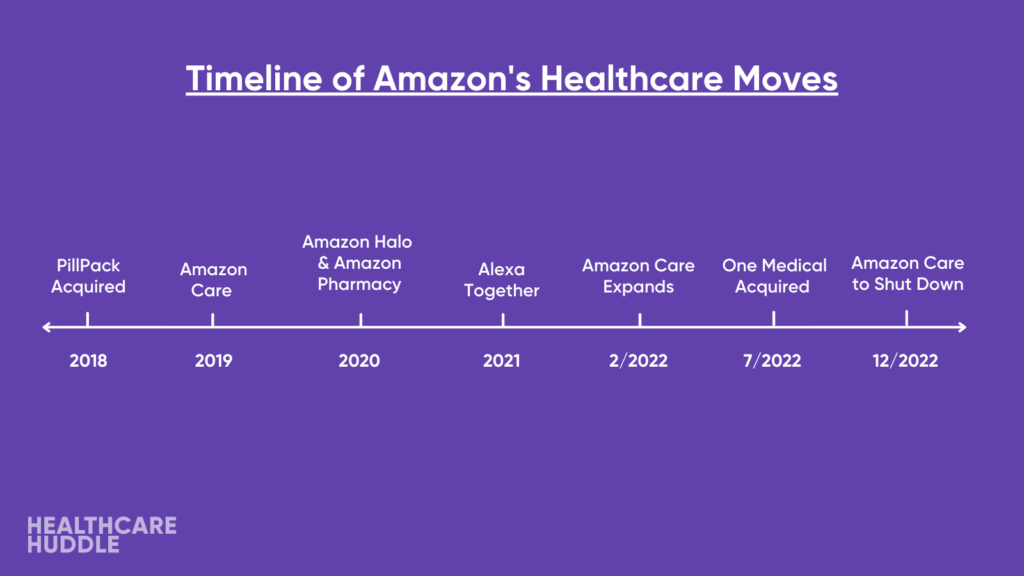
There’s a lot of chatter regarding what’s next for Amazon in the healthcare world. Some think their next move will be acquiring an insurance company or health system. Only time will tell.
CVS Acquires Signify Health for $8 Billion
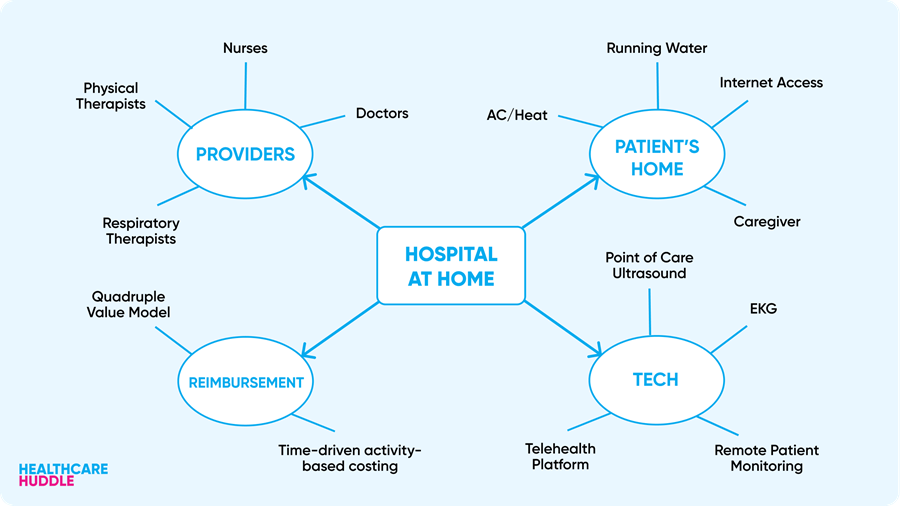
CVS Health outbid Amazon and UnitedHealth Group to acquire home health company Signify Health for $8 billion. This acquisition will give CVS Health access to Signify’s 10,000 clinicians in all 50 states, technology to coordinate care and nearly 2.5 million homes (read: a good referral stream to other CVS Health services). Additionally, CVS will gain access to Caravan Health, an ACO company acquired by Signify. Caravan has 170 Medicare providers covering 700,000 patients. CVS’s acquisition of Signify Health supports a new movement in healthcare, what many are calling the healthcare at home renaissance.
I first wrote about healthcare at home back in January when MyMichigan Health announced it would officially launch a hospital-at-home program. The health system joined 100+ other U.S. hospitals that are trying to deliver high-value care.
While hospital-at-home programs allow for intensive care in the comfort of the patient’s home, general health care at-home programs (like Signify) allow for preventative, routine care, still in the comfort of patients’ homes.
Updated Covid-19 Booster Vaccine
The FDA approved Pfizer and Moderna’s updated Covid-19 booster vaccine, which provides protection against the dominant BA.5 omicron subvariant. The government purchased 175 million of these updated vaccines for around $5B (105 million doses from Pfizer for $3.2 billion and 66 million doses from Moderna for $1.74 billion). Both of these companies had a profitable year in 2021 (I covered Pfizer here). Pfizer and Moderna will continue to form contracts with other governments to purchase their updated vaccines, and it’s likely the best option they have, considering the rate of booster uptake in the U.S. is abysmal compared to peer nations, coming in at 33%.
Dive Deeper:
- Amazon to Acquire One Medical for $3.8 Billion
- CVS Acquires Signify Health for $8 Billion
- FDA to Approve Omicron Booster
If you enjoyed this recap, share it with colleagues. Sign up for the Healthcare Huddle newsletter here.