24 September 2022 | Healthcare
How to Fix the Postpartum Insurance Cliff
By workweek
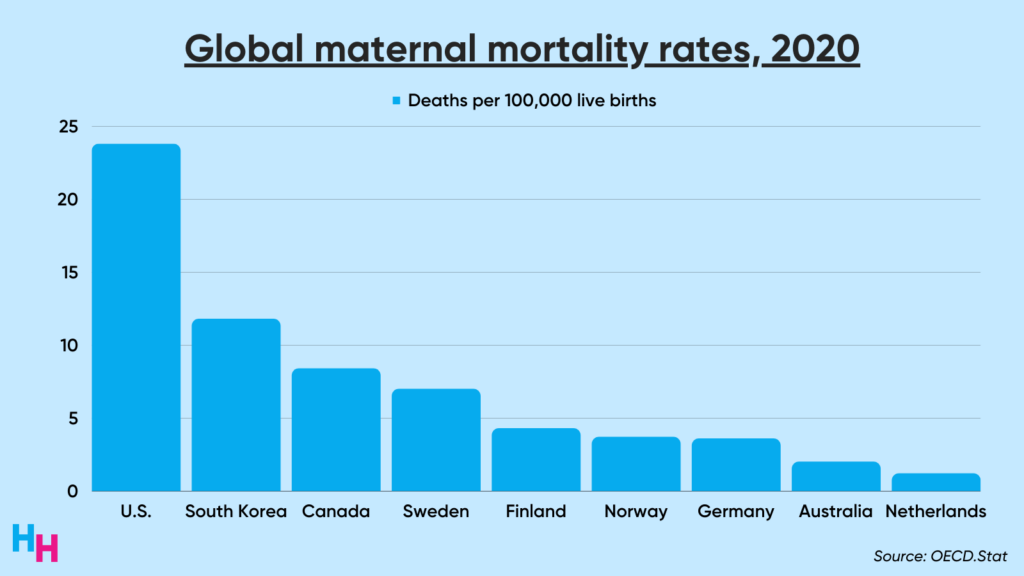
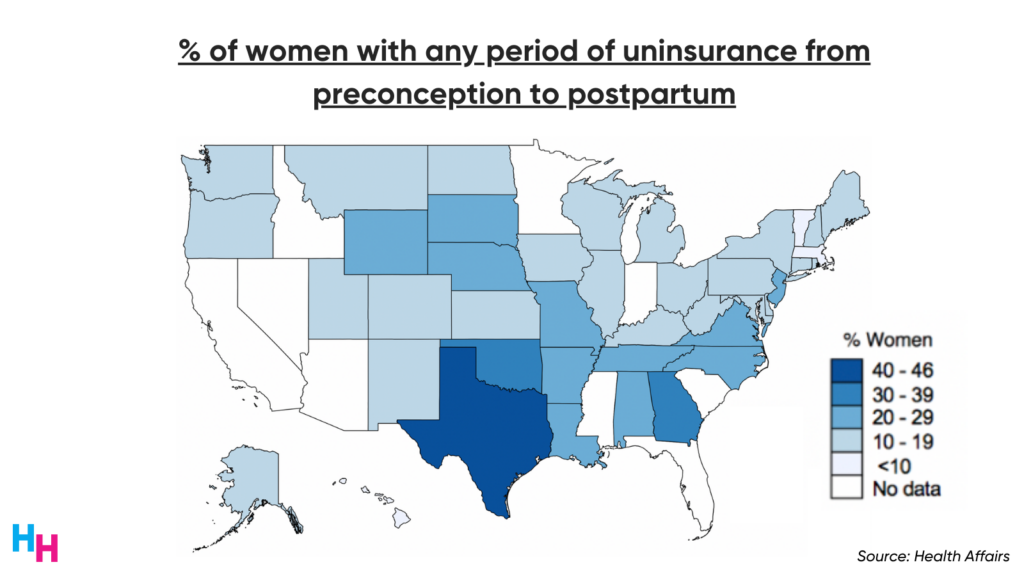
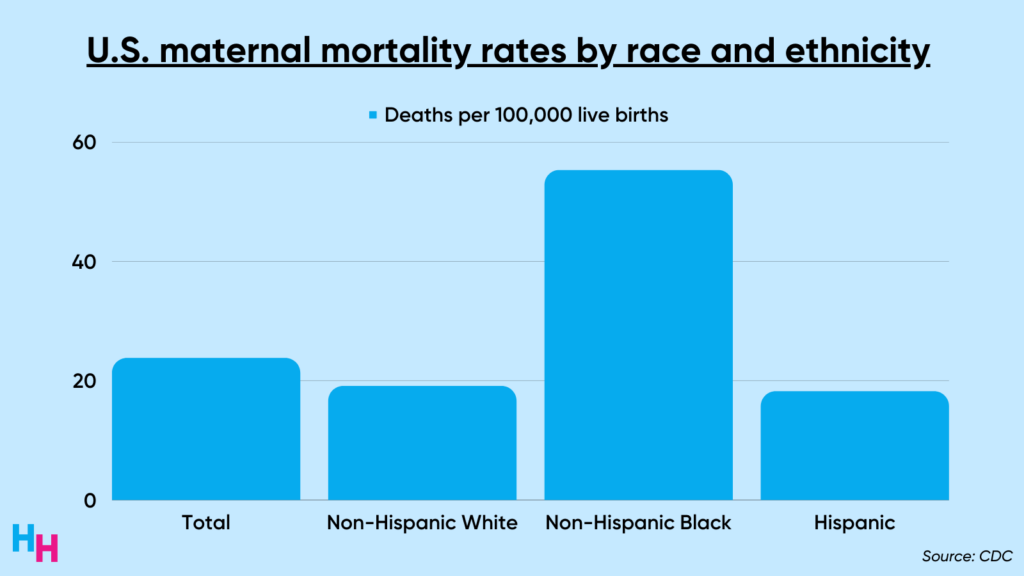
Insurance coverage and maternal health outcomes in the U.S. trail behind peer nations. One study found one in five women lost insurance coverage throughout the preconception, prenatal, peripartum and postpartum periods. With insufficient insurance access throughout pregnancy, is it a surprise, then, that 24 mothers die for every 100,000 live births in the U.S.?
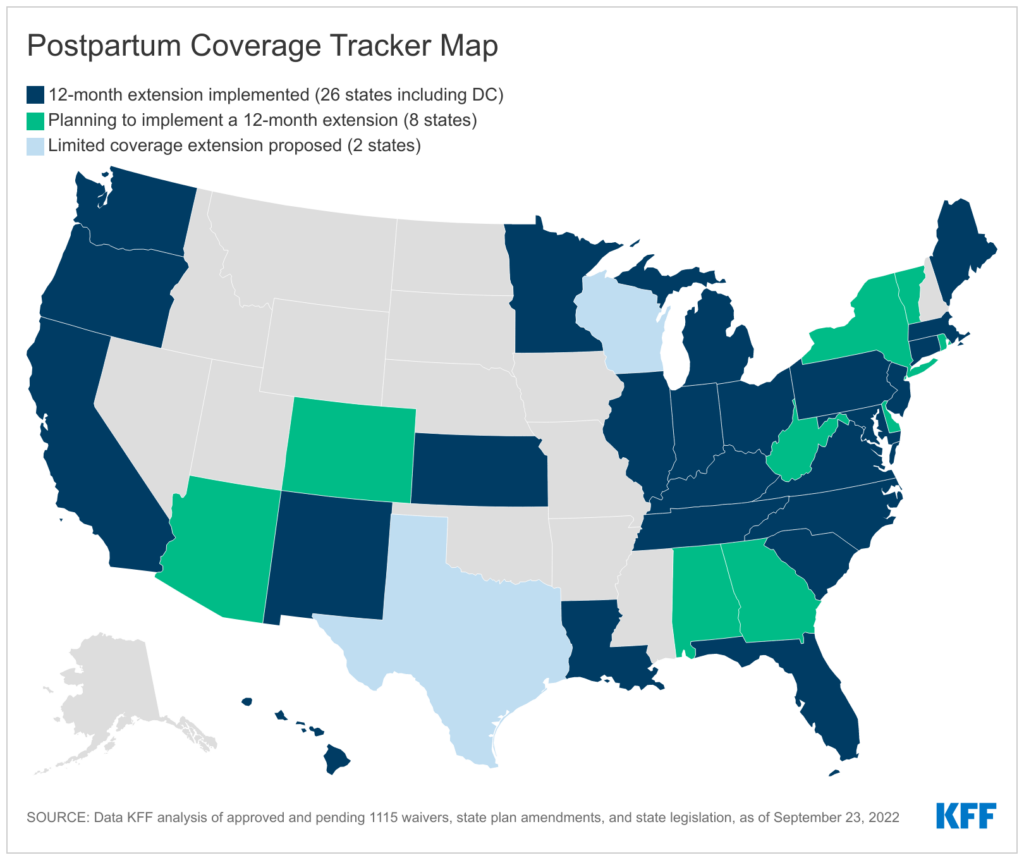
Lawmakers have attempted to address insurance coverage and postpartum outcomes through policy changes. For example, thirty-four states have implemented or plan to implement a 12-month Medicaid extension for postpartum women allowed through the American Rescue Plan Act (ARPA). Standard postpartum Medicaid coverage lasts only 60 days after delivery. Following 60 days, the mother is booted from Medicaid if they do not qualify based on income.
The ARPA is the solution needed to address insurance coverage lapses during the postpartum period, improving postpartum outcomes such as maternal mortality.
The Problem
Federal law requires states to provide pregnancy-related Medicaid coverage for up to 60 days postpartum. Note, this coverage provides pregnancy-related Medicaid benefits—not full Medicaid benefits. Fortunately, income restrictions for pregnant women to qualify for Medicaid are more lenient than those for parents. For example, in Texas, pregnant women whose income is 207% of the federal poverty level (FPL) qualify for Medicaid coverage while parents whose income exceeds 17% of the FPL do not qualify.
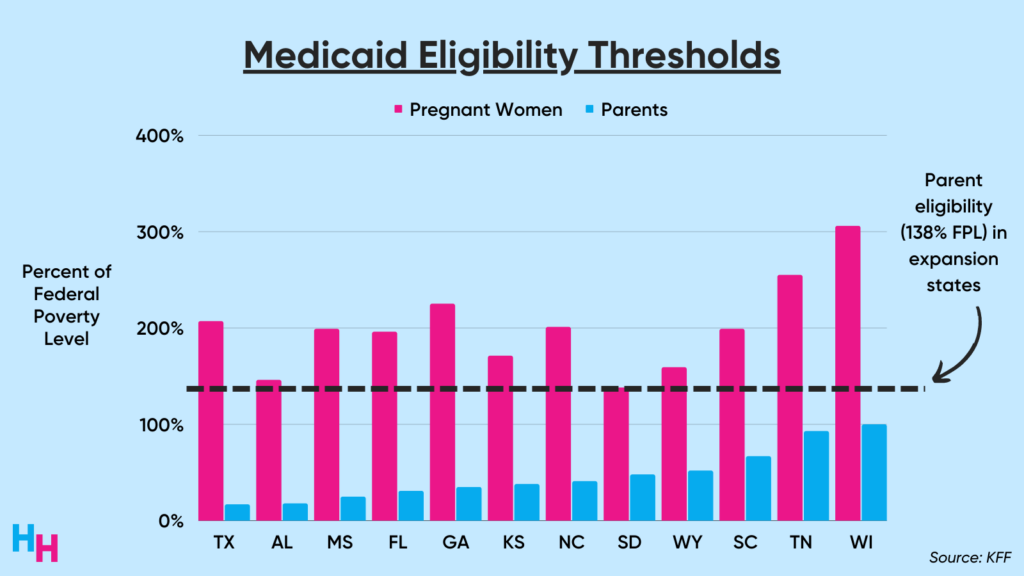
After 60 days postpartum, many new mothers face a dooming insurance cliff—especially those in states that have not expanded Medicaid, like Texas. If a new mother’s income is greater than the maximum income needed to qualify for Medicaid, then they’ll lose insurance coverage. So, if you’re a Texan mother with an income 100% of the FPL, Texas’s Medicaid program would cover you until 60 days postpartum and then drop you.
Gain of insurance followed by loss of insurance is known as churn. As you’d expect, non-expansion states have higher churn rates for women during the prenatal, peripartum and postpartum periods. Texas has the highest churn rate.
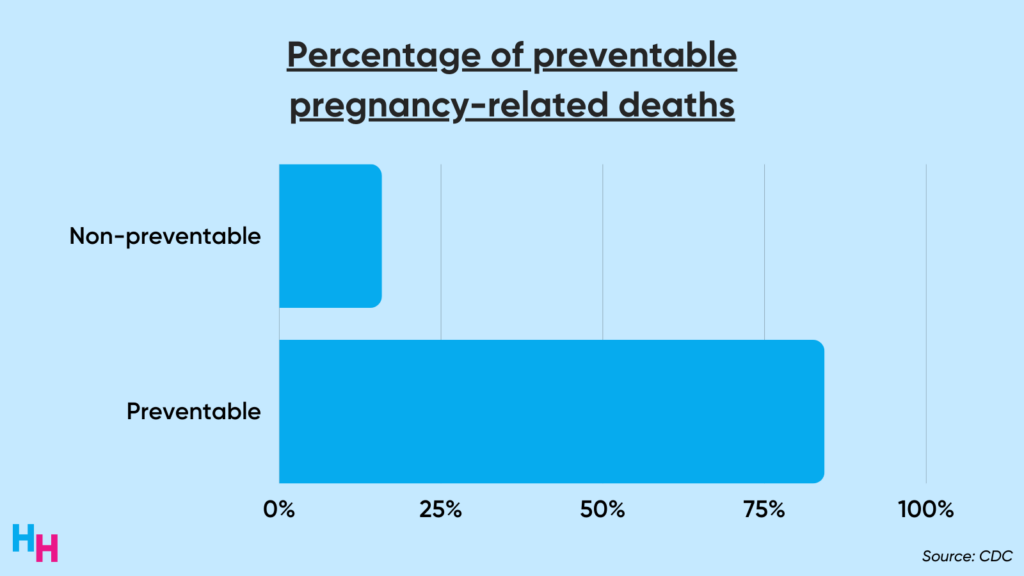
Churn is dangerous for pregnant and postpartum women, as it leads to poor continuity of care, delaying prevention, diagnosis and treatment of diseases or complications that can result in death. One in three pregnancy-related deaths occurs between one week and one year postpartum, but 85% of those deaths are preventable. “Preventable death,” as defined by the CDC study, is “at least some chance of the death being averted by one or more reasonable changes to patient, community, provider, facility, and/or systems factors.” Insurance coverage, therefore, prevents death.
The Solution
The American Rescue Plan Act signed in 2021 provided states the option to extend Medicaid postpartum coverage from 60 days to 12 months after delivery in return for increased Medicaid funding. The extension, which began April 1st, 2022, provides full Medicaid benefits, not just pregnancy-related benefits. The funding for the postpartum Medicaid extension is set to expire in 2027, costing the government $6.1 billion over 10 years. Therefore, we face another insurance cliff, which I discussed last week, although this one is half a decade away.
Thirty-four states have implemented or plan to implement Medicaid postpartum coverage extension, including conservative states like Florida, Louisiana, Alabama and Missouri. If all states were to adopt the Medicaid postpartum coverage extension, then 720,000 people would be guaranteed insurance coverage for a full year after delivery.
We likely won’t see the benefits of the ARPA’s Medicaid postpartum coverage extension until after the public health emergency ends. If you recall from last week’s article, the Family First Coronavirus Response Act required states to provide continuous Medicaid enrollment, meaning if your income surpasses the qualifying income for Medicaid, you’ll maintain your insurance instead of losing it. Therefore, all women who qualified for Medicaid while pregnant have retained insurance throughout the prenatal, peripartum and postpartum periods.
However, continuous enrollment will end as soon as the public health emergency ends—which will be soon. Only then will we see the ARPA’s work in action.
Dash’s Dissection
I predict we’ll see maternal mortality rates decrease in 2021 and 2022 because of continuous enrollment, allowing thousands of mothers to have maintained Medicaid insurance throughout the entire length of their pregnancy and postpartum period. In fact, we saw maternal mortality rates decrease by 7 deaths per 100,000 live births in states that expanded Medicaid coverage vs states that did not expand Medicaid coverage. Simply put, insurance coverage is a determinant of maternal health.
However, after the public health emergency ends, I expect states that did not extend postpartum Medicaid coverage to experience poorer maternal health outcomes than those that did extend coverage. And remember, maternal mortality does not affect everyone equally. The maternal mortality rate for non-Hispanic Black mothers is nearly 3x higher than non-Hispanic white mothers.
How we incentivize all states to extend postpartum Medicaid coverage is a multi-billion dollar question. Perhaps we should skip the incentive and go straight to a mandate. Several Democrats are writing legislation that would mandate all states to extend postpartum Medicaid coverage after failing to do so in the Inflation Reduction Act. They want to fit it into an omnibus appropriations package for next year. I’m doubtful that this will happen, given we couldn’t even mandate all states to expand Medicaid. However, such an extension of Medicaid coverage may give conservative states who outright banned abortion an opportunity to say, “Hey, we actually care about women’s health, so we’ve extended postpartum Medicaid coverage.” But this is likely wishful thinking.
Maternal health is a major weakness of the U.S. healthcare system. The ARPA has significant potential to improve maternal health by allowing states to extend postpartum Medicaid coverage from 60 days to 12 months. While funding for extending coverage will last five years, that’s sufficient time to realize the benefits of maintaining insurance coverage throughout the entire preconception and postpartum journey.