22 April 2023 | Healthcare
The Affordable Care Act: Facing a New Legal Challenge on Preventive Care Coverage
By workweek
The Affordable Care Act (ACA) has weathered over 2,000 lawsuits aimed at dismantling or completely eliminating the legislation. Despite this onslaught, the ACA has remained resilient.
However, the ACA now faces a fresh challenge as it re-enters the legal arena.
District Court Judge Reed O’Connor recently struck down a critical provision of the ACA, which mandates that nearly all private health plans cover preventive services without any cost-sharing. The federal government has already appealed the decision.
In this article, I will explore the ACA’s requirement for coverage of preventive services, examine the lawsuit that seeks to undermine this provision, and evaluate the consequences if it’s ultimately repealed.
Background on Cost-free Preventive Services
Section 2713 of the ACA requires all private health plans to cover preventive care services with zero cost-sharing, except for around 13% of those plans with “grandfathered” status. Such a status exempts health plans that were in effect before the ACA was passed.
To decide which preventive services private health plans must provide with zero cost-sharing, Congress assigned three expert clinical and scientific entities:
- U.S. Preventive Services Task Force (USPSTF): recommends evidence-based care for infants, children, and adults. They rank the evidence with a letter grade from A to I. Health plans must cover preventive services with an evidence-based rating of A or B, meaning there is high certainty the rendered services have a substantial or moderate net health benefit.
- Advisory Committee on Immunization Practices (ACIP): develops recommendations on immunizations.
- Health Resources and Services Administration (HRSA): recommends preventive services for children (Bright Futures for Children) as well as certain services for women (Women’s Preventive Services Initiative).
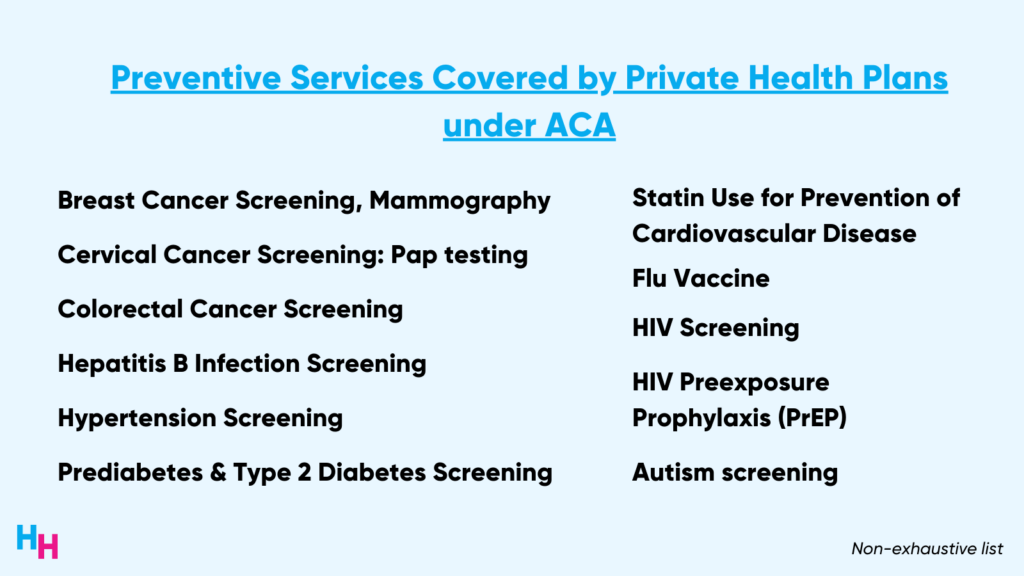
Below is a non-exhaustive list of the nearly 200 basic preventive services health plans must cover with zero cost-sharing. Note that colon cancer screening, PrEP for HIV prevention, and contraceptive coverage are included.
The Lawsuit: Braidwood Management Inc. v. Becerra
Brainwood Management Inc, along with several individuals and businesses (” plaintiffs”), filed a lawsuit alleging that the ACA’s mandate for preventive care coverage has caused economic and religious harm. They claim that they do not require or desire certain preventive services and that some of the mandated services conflict with their Christian and moral beliefs.
In September 2022, the case was brought to Judge Reed O’Connor at the U.S. District Court in the Northern District of Texas, who made the final ruling in March of this year:
- Private health plans are not required to provide cost-free preventive services recommended or updated by USPSTF on or after March 23, 2010 (when the ACA was enacted).
- The PrEP coverage requirement for HIV prevention violates the plaintiffs’ religious/moral beliefs and objections.
First, Judge O’Connor ruled that the ACA’s delegation of authority to the USPSTF to determine which preventive health services health plans must cover violates the Appointments Clause of the Constitution. According to the Appointments Clause, the President appoints federal officers, and the Senate confirms them. The plaintiffs argued the expert entities involved in this case are federal officers due to their significant decision-making power, yet they were not appointed by the President, which violates the Appointments Clause.
Judge O’Connor agreed with the plaintiffs, but ruled that delegating to USPSTF violates the Appointments Clause—not the other entities. USPSTF recommendations are not subject to the oversight or approval from a governing body while ACIP and HRSA recommendations are subject to such oversight by the Secretary of HHS, for example.
Second, Judge O’Connor ruled the requirement to cover PrEP for HIV prevention violates the Religious Freedom Restoration Act. The plaintiffs originally argued that PrEP coverage violates their religious beliefs by promoting “homosexual behavior, prostitution, sexual promiscuity, and intravenous drug use.”
The federal government has appealed Judge O’Connor’s decision to the U.S. Court of Appeals for the 5th Circuit. Whether Judge O’Connor’s ruling will be blocked while the appeal happens is TBD.
Dash’s Dissection
The impact of Judge O’Connor’s ruling will be profound if it stands, affecting the 60% of Americans with private health plans providing cost-free preventive services.
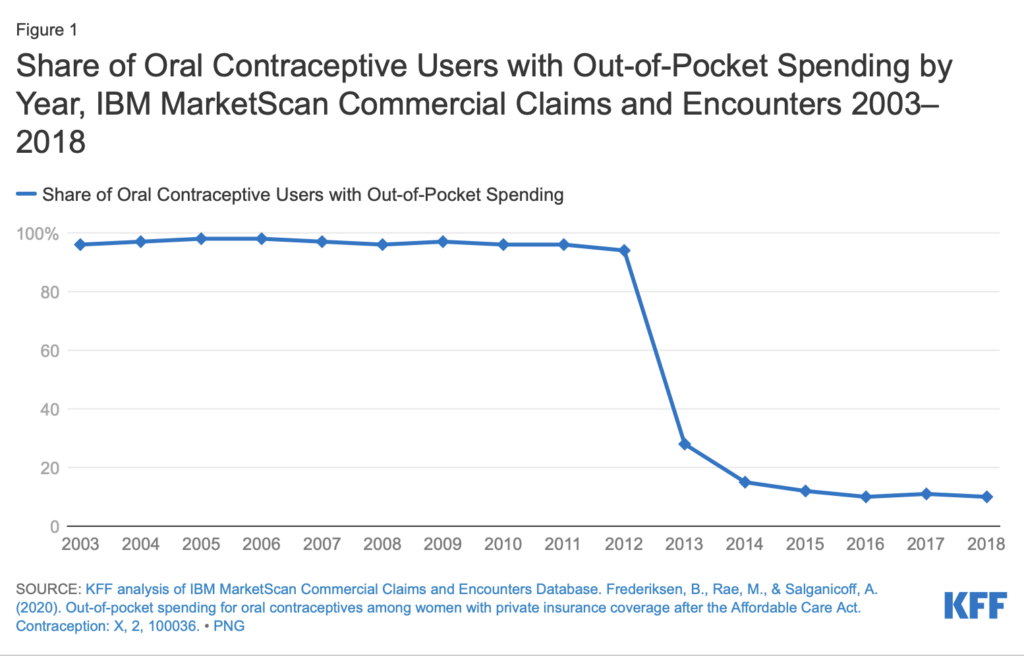
People are less likely to use preventive care services if they have to pay for it. That’s why we’ve seen a notable increase in colorectal cancer screening tests, immunizations (e.g. HPV vaccine), Medicare annual wellness visits, and prescription contraceptive usage since the start of the preventive care provision. Below, you can see the drop in the proportion of oral contraceptive users’ out-of-pocket spending after the preventive services provision was enacted.
Note again these preventive services are backed by strong evidence that such services will provide substantial health benefits with moderate or high certainty. Colorectal cancer screening, for example, averts 24-28 deaths per 1,000 screenings for 45-75-year-olds; cervical cancer screenings have contributed to a 75% decrease in incidence and mortality since the screening’s introduction in the 1960s; PrEP reduces HIV risk from sexual transmission by nearly 99% and IV drug use by at least 74%.
Removal of cost-free coverage of preventive services will therefore have a profound impact on population health and exacerbate health inequities. For example, while breast cancer screenings remained stable after the ACA’s enactment, it increased among Black women, helping close the racial gap in screening mammography. Removal of cost-free mammography may reverse this progress. Additionally, over 80% of the 80,000 individuals taking PrEP (cost-free) have commercial insurance. Removing coverage will have a significant impact on access and cost (PrEP is $30/mo), exacerbating health disparities among LGBTQ+ populations.
The ACA’s preventive services framework is hanging by a thread, and if cut, will truly disrupt patient care. While USPSTF is an independent body of experts, it does hold significant decision power that impacts all Americans and legally requires “sensible checks and balances,” as demonstrated in Judge O’Connor’s ruling. The Biden administration and Congress need to intervene now before it’s too late. Here are some options to add (legally) needed oversight to USPSTF:
- Authorize the director of AHRQ or CDC to review and implement USPSTF’s recommendations.
- Establish another division within HHS to review, implement, or reject USPSTF’s recommendations.
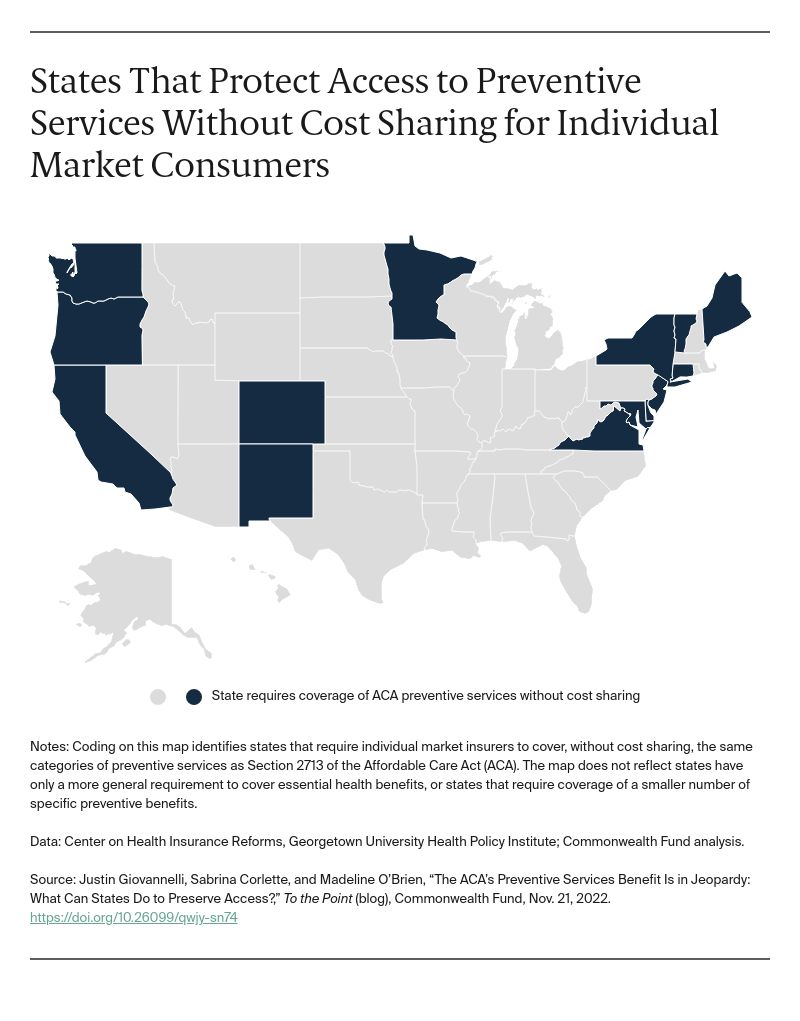
If this doesn’t work out, then states can implement their own ACA-like preventive services at zero cost-sharing. Fifteen states have already done so.
In summary, the Affordable Care Act is currently facing a new legal challenge, as District Court Judge Reed O’Connor has struck down the mandate for cost-free preventive care coverage. This decision, if upheld, could have far-reaching consequences for millions of Americans who rely on private health plans for preventive services. The ruling threatens to exacerbate poor health outcomes, health disparities, and health inequities by reducing access to evidence-based preventive care. The federal government has appealed the decision, and the outcome remains uncertain. In the meantime, the Biden administration and Congress, as well as individual states, should explore potential solutions to maintain access to cost-free preventive care and ensure the continued positive impact of the Affordable Care Act on the health of the nation.
OUTSIDE THE HUDDLE
1) Supreme Court Rules on Mifepristone Availability During Lawsuit
SCOTUS ruled to maintain the status quo on mifepristone availability—which includes access to the medication by mail order—while a lawsuit challenging mifepristone plays out in the lower court. Here’s a quick timeline of the events surrounding mifepristone:
- November 18, ’22: Alliance Defending Freedom (a group that opposed abortion) accused FDA of illegally rolling back restrictions on mifepristone over the years. They seek to reverse mifepristone’s FDA approval for abortion.
- April 7, ’23: U.S. District Judge ruled in favor of Alliance Defending Freedom, issued order to block sales of mifepristone nationwide.
- April 12, ’23: U.S. Fifth Circuit Court of Appeals blocked part of District Judge’s order, allowing for mifepristone to remain on market, but with stringent restrictions on access (e.g., blocking mail order, requiring physician visit, suspending generic version).
- April 13, ’23: Justice Department and Danco Laboratories (mifepristone distributor) sent emergency request to SCOTUS, the company that distributes mifepristone.
- April 22, ’23: SCOTUS ordered mifepristone to remain widely available while lawsuit continues in lower court.
- May 17, ’23: U.S. 5th Circuit Court of Appeals will hear oral arguments.
2) Teledoc Enters Weight Management Space (I’m not surprised)
Teledoc announced it’s expanding its Provider-Based Care to weight management and prediabetes. At this point, you shouldn’t have to guess why Teledoc is moving into weight management now vs starting there as soon as they launched their Provider-Based Care for diabetes and hypertension. The weight management market is hot (dare I say, “on fire”?) with these GLP-1 agonists. Teledoc is just following its competition. I predicted this would happen back in February:
Established virtual care startups will start launching new weight-management services, and new virtual care startups will follow suit.
Read my article here: Do Weight-management Startups Have a Future? Next week’s Huddle will be on these weight management companies, so stay tuned!
3) Mark Cuban’s Cost Plus Drugs Now Partnering with Independent Pharmacies
Cost Plus Drugs announced it will partner with over 30 pharmacies nationwide that will accept a discount card (” Team Cuban Card“) to help patients purchase their medications at lower prices. This move will help Cost Plus Drugs compete with GoodRx and also help support independent pharmacies that incumbent PBMs and pharmacies have been trying to wipe out. Listen to Cost Plus Drugs CEO Alex Oshmyansky’s interview at Yahoo News where he discusses how Cost Plus Drugs will support independent pharmacies. Cost Plus Drugs is moving quickly… I’m going to have to write a mid-year update! Read my previous update here.
If you enjoyed this deep dive, share it with colleagues. Sign up for the Healthcare Huddle newsletter here.