20 August 2022 | Healthcare
How to Make Outpatient Scheduling More Efficient
By workweek
An appointment with my dermatologist—that’s who I’m waiting for.
I called my dermatologist’s office to make an appointment for a routine body check, hoping to get an appointment in a week or two.
“A week or two? The next available appointment is in three months. Which day works best for you?”
“But… I don’t know what my schedule will be in three months. ”
“Perfect… we’ll just schedule you in whenever then.”
That’s three months between scheduling my appointment to my actual appointment date, what’s known as a lead time. You likely understand the frustration of scheduling a timely appointment with a specialist.
I’m all about efficiency and effectiveness—I see my world through the lens of process maps. So, during my Master’s program in Healthcare Systems Engineering in 2019, my best friend and fellow Huddler, Jonny Blum, and I set out to understand why it takes so long to schedule an appointment with a specialist and what we can do about it.
The Deets
Let’s talk about a perfect reality:
- There are no appointment cancellations
- There are no no-shows
- There are no walk-ins (since there are no free openings if each patient arrives on time, as scheduled).
- The physician takes advantage of the full-time slot allocated for each patient.
In *our* reality, 10% of patients fail to show up to their scheduled appointments and 20% of patients cancel their scheduled appointments. Despite the number of appointments that become available from such no-shows and cancellations, patients wait on average 24-days to obtain an appointment. This wait time may exceed 100 days depending on the market size.
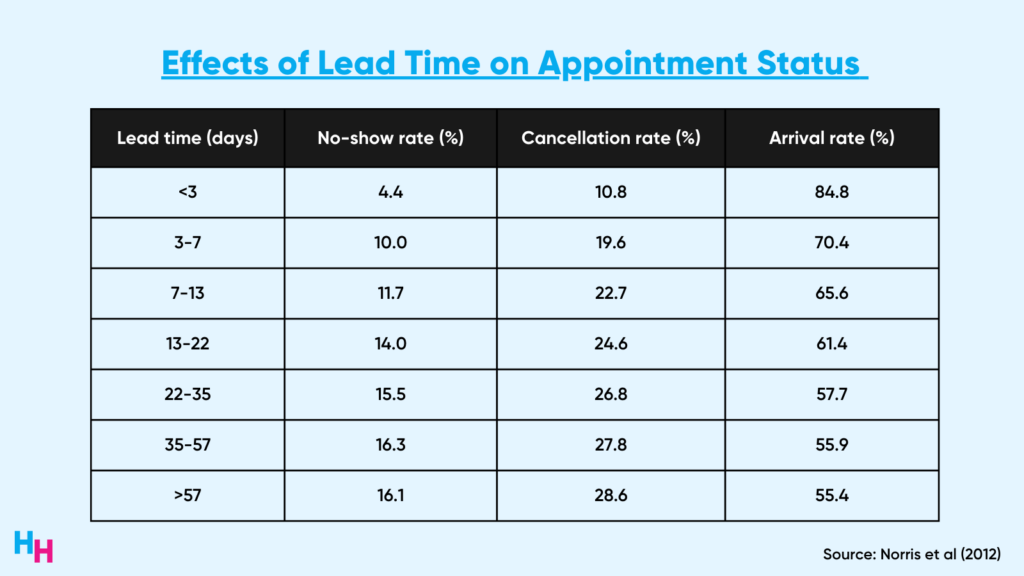
The irony is that there’s a positive correlation between cancellations/no-shows and lengthy lead times. That is, offices that schedule patients far in advance to fill future slots are actually doing a disservice because longer lead times increase the chances of no-shows and cancellations. For example, a lead time of over 55 days results in a 16% no-show rate and 29% cancellation rate.
In reality, the efficiency and utilization of obtaining a reasonable appointment time within the U.S. healthcare system is far from an ideal scenario.
So What?
Patients and doctors experience significant negative consequences of cancellations, no-shows and long wait times to schedule appointments. Long wait times to schedule an appointment for specialty care are associated with lower compliance, worse medical outcomes and increased patient dissatisfaction.
For physicians, no-shows and cancellations lead to decreased efficiency in the practice. In one study by Moore and colleagues (2001), over the course of the year, revenue shortfalls due to cancellations and no-shows at a practice could range from 3%, assuming replacement of all scheduled patients by walk-ins, to 14%, assuming the level of replacement encountered in this study. The projected loss of revenue across 250 working days per year would be more than $350,000. Now, imagine how large this number would be if all clinics in the U.S. were included.
Current Solutions
Jonny and I interviewed dozens of specialty practices, ranging from dermatology to ENT, to better understand their scheduling processes. The lead times ranged from two weeks to six months and each office reported that daily no-shows and cancellations were the norms. When we asked how they deal with patients wanting earlier appointments, they said they maintain a waitlist.
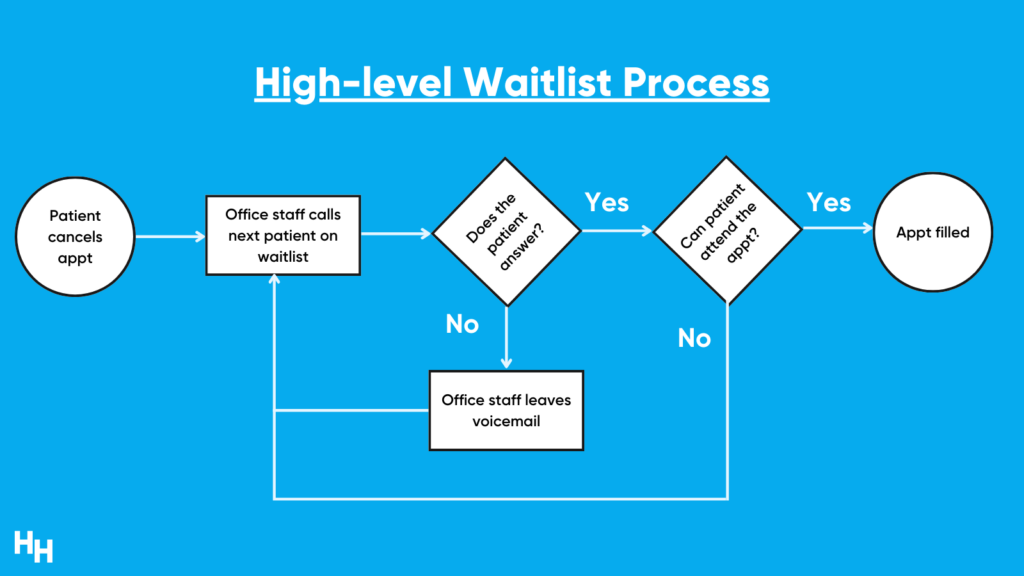
These waitlists varied from excel spreadsheets to paper binders where the office staff would write down the patient’s name and phone number. When there was a cancellation or no-show, the office would go to their waitlist and successively call the patients on it. No answer? Leave a voicemail and proceed to the next patient until one of them answers and confirms the new appointment. This is absurdly inefficient.
Solution
There are a couple of root causes of the no-show and cancellation problem, depending on the perspective you’re analyzing: the patient or the office. Jonny and I focused on no-shows/cancellations accompanied by pages-long waitlists from the office’s perspective.
The solution I want to focus on is automating the manual waitlist process. That is, office staff working their way through long waitlists to call patients to fill in new openings. The automation entails sending automated text messages to patients on the waitlist as soon as a no-show or cancellation occurs. After five minutes of no answer from the patient on the waitlist, the next patient in line receives the text message, and so forth.
Regarding technicalities, the automation can work as a standalone platform or integrate into the EHR. The former may add minimally more friction to the workflow of the office staff while the latter would require substantial investor funding to build a team of engineers (trust me, we looked deep into this).
Jonny and I created a simulation model to demonstrate the financial consequences of no-shows and cancellations based on data from the literature and the effects of automation. You can access the model on your computer and play around with it by clicking the button below (please make a copy of the Google Sheet).
Within the model, comments are embedded in the cells to elaborate on certain calculations and definitions. Additionally, any italicized and underlined cell is hyperlinked to the “Assumptions” tab. Anyone experimenting with this model can manipulate the inputs on the “Dashboard” tab. Changing the inputs will change the values shown in the graphs.
Automating the process gives patients quicker access to health care while filling in openings in the office’s schedule that would have been otherwise vacant. Compared to baseline data for a typical dermatology office (see image below for some assumptions made), automating the waitlist process can decrease time spent on reminder calls by the office staff from 160 hours to under 20 hours annually. Additionally, since this model assumes automation is effective at filling in open appointments with patients who want earlier ones, 95% of all appointments will be filled and recovered, resulting in a $250,000 revenue increase annually.
There are a handful of companies tackling this inefficiency. Give them a look:
- Luma Health
- NexHealth
- QueueDr (acq by Phreesia)
Take Home Message
There are more inefficiencies in the U.S. healthcare system than there are cockroaches in New York City.
- If you don’t believe there could be so many cockroaches in NYC, then you have a solid understanding of this healthcare system.
- However, if you don’t believe there could be so many inefficiencies in this system, then you need to visit NYC.
P.S.
Investigating patient wait times and inefficiencies was part of my capstone project at Lehigh University during my master’s program in Healthcare Systems Engineering. It was destined to turn into a full time venture called Nayroo, but once I started medical school, I quickly learned how hard it’d be to balance studies and operations. So, we had to put Nayroo on the shelf.
Either way, I learned so much about this healthcare system through the program and the capstone project—there would be no Healthcare Huddle without this program… think about that for a second.
Many thanks to my professors who advised on the project, Professors Ana Alexandrescu, Terry Theman, Robert McDonald.
And of course, I need to shout out Jonny Blum, Lewis Lazarus, Dan Berkowitz and Adam Sugarman who all played essential roles in the research and prototyping of the project, Nayroo.
Dive Deeper
- An empirical investigation into factors affecting patient cancellations and no-shows at outpatient clinics (link).
- Waiting Your Turn: Wait Times for Health Care in Canada, 2020 Report (link).
- Prevalence, predictors and economic consequences of no-shows (link).
- Appointment scheduling in health care: Challenges and opportunities (link).
- Sick of waiting: Does waiting for elective treatment cause sickness absence? (link).