06 August 2022 | Healthcare
Graying America and the Geriatrician Shortage
By workweek
As my anatomy professor used to say, aging is inevitable and beautiful. But, to ensure we age beautifully, we need the right people to help us—which is the big problem.
While the population of adults 65 and older continues to grow, the population of geriatricians—physicians specialized in caring for the complex needs of older adults—isn’t growing quickly enough.
Despite the attractive work-life balance of geriatricians, few physician residents choose to specialize in the field. Subpar reimbursement and extra year(s) of training are likely to blame. So, what can we do about the geriatrician shortage?
Geriatrics 101
The study of “old age” dates back to Greek mythology. The Gods sent Pandora and her box to civilization to punish humanity for Prometheus stealing fire from them. As everyone does when they see a fancy box, they open it. Inside Pandora’s box were plagues, diseases and—most important—old age.
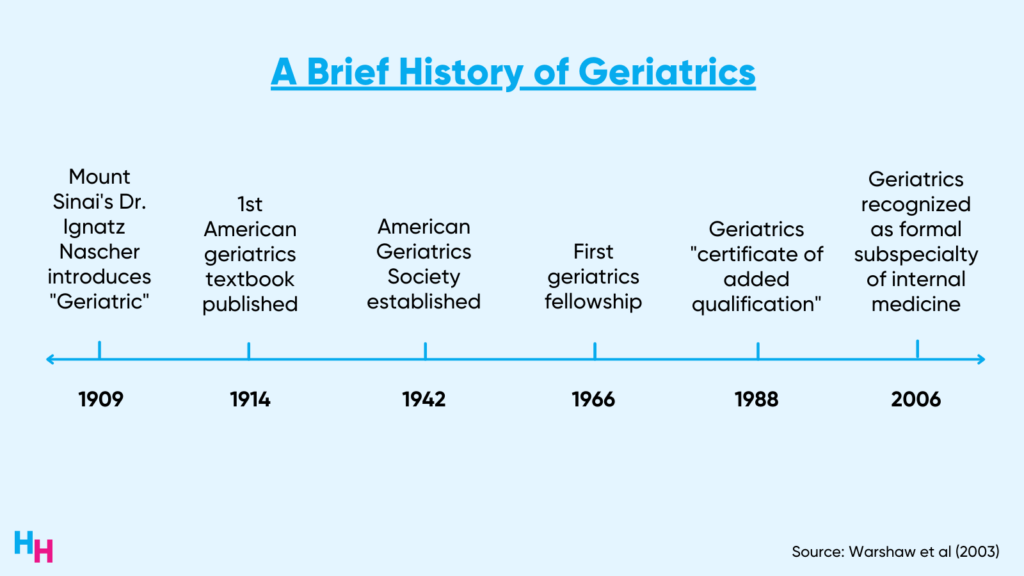
Fast forward to 1966 when Dr. Leslie Libow created the first fellowship in geriatric medicine at a Mount Sinai hospital. Geriatrics is a specialized field of internal medicine focused on identifying the asymptomatic and atypical presentations of disease in older adults. Most importantly, Geriatricians are experts at managing the 5Ms: mind, mobility, medications, multi-complexity and what matters most.
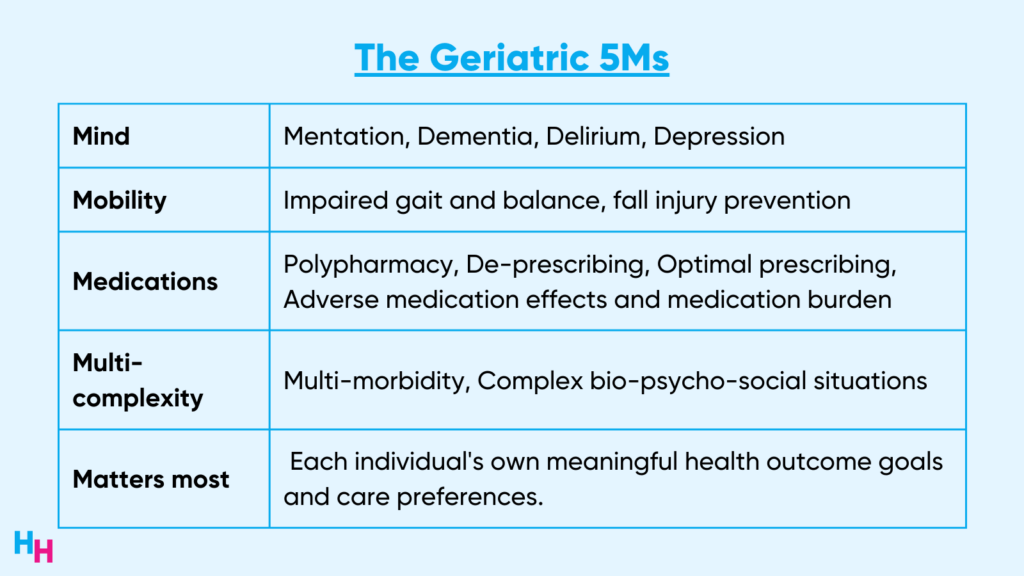
These areas are critical to managing the health of older adults, especially those with complex illnesses and needs. It’s estimated that 30% of the 78 million baby boomers will require specialized geriatric care.
Since Dr. Libow’s launch of the inaugural geriatrics fellowship, hundreds of academic institutions have established their geriatric fellowships. In 1988, physicians could subspecialize in geriatrics by earning a “certificate of added qualification.” Resident physicians could either complete a fellowship or “practice experience pathway” to obtain such a certificate.
However, in 1994, the “practice pathway” was phased out, and a two-year fellowship in geriatrics was required to specialize in the field. This fellowship was then shortened to one year in 1998 after fewer and fewer resident physicians chose geriatrics. Finally, in 2006, the American Board of Internal Medicine formally recognized geriatrics as a subspecialty of internal medicine instead of a certificate of added qualifications.
Despite the formal recognition of the subspecialty, geriatrics subspecialization has failed to gain traction.
The Shortage
Estimates suggest we need 30,000 geriatricians to optimally care for the 30% of 78 million boomers needing specialized care by 2030. There are a couple of problems:
- 2030 is just seven years away.
- There are currently only 7,300 geriatricians.
- Half of these geriatricians work part-time.
So, there’s around one geriatrician per 10,000 older adults when we actually need one geriatrician per 700 older adults. We’re nowhere close to that. And it looks like it’ll stay that way.
From 2014 to 2017, the number of ACGME-accredited geriatric fellowship spots declined from 509 to 478. Then, in 2017, only a quarter of the 141 fellowship programs were filled for all positions, leaving 222 positions unmatched. So, while the population of adults 65 and older is expected to grow 17% from 56 million today to 95 million by 2060, the growth of geriatricians appears stagnant.
Despite the highest career satisfaction, geriatrics doesn’t attract enough medical students or resident physicians. Likely, the most significant reason is low pay. Geriatrics is the 4th lowest paid specialty. In fact, as a geriatrician, you make on average $20,000 less than a general internist. That’s an additional year of training and not being paid a physician’s salary only to make less than you would by not going into geriatrics. Do you see the problem? Additional issues include lack of exposure to geriatrics during medical school, mentorship, financial rewards and prestige.
Three Potential Solutions
The root cause of all problems in healthcare is money. Therefore, financial incentives are the first steps to incentivizing medical students to choose a career in geriatrics.
The first solution that comes to mind is student loan forgiveness. Programs are already implementing student loan forgiveness to incentivize careers in primary care or work in rural areas. Such programs have shown some success. As such, a student loan forgiveness program for geriatrics may show similar success. In this case, students would commit to an internal medicine residency followed by a one-year fellowship in geriatrics.
An additional financial incentive would be private practice start-up funding. I predict we’ll see a shift from the employed hospital physician to the private practice physician, meaning more doctors will need help starting their practices. For example, the government could create a program that covers a private practice’s start-up costs, including technology, staff, equipment and office space. Perhaps the government partners with startup companies like Ease, which helps physicians startup their private practices.
Lastly, increased exposure to geriatrics may pique medical students’ interest in the field early in their medical education. For example, schools like the Icahn School of Medicine have the Medical Student Training in Aging (MSTAR) program. This program, sponsored by the National Institute on Aging, encourages medical students early on to pursue research in aging and palliative medicine through short-term scholarships. The research opportunities span health services, clinical trials and basic science. Anecdotally, I’ve only heard great reviews of the program.
Another way medical students can gain exposure to geriatrics is through an established geriatrics clerkship curriculum. Again, speaking from personal experience, the Icahn School of Medicine has a three-week geriatrics and palliative care curriculum where students rotate in outpatient and inpatient settings, learning how to manage older adults’ complex needs. While three weeks isn’t necessarily long, it was sufficient to provide that early exposure and insights into geriatrics.
Conclusion
Thirty percent of the 78 million boomers will need specialized geriatric care by 2030. To optimally care for this population, we’ll need around one geriatrician per 700 older adults. However, there’s currently only around one geriatrician per 10,000 older adults. This is a problem.
Several solutions address the geriatrician shortage, including financial incentives and early exposure during medical training. Overall, a multi-modal solution is likely needed to fix the geriatrician shortage.