02 July 2022 | Healthcare
Healthcare Q2 ’22 Recap
By workweek
BUSINESS
The Netflix of Antibiotics
The UK plans to use a subscription-based model for Pfizer and Shionogi to increase the supply of powerful antibiotics. The UK government will pay the two companies $13M/year over the decade for a guaranteed supply of two drugs, cefiderocol and ceftazidime-avibactam. This subscription model is known as a “pull incentive.”
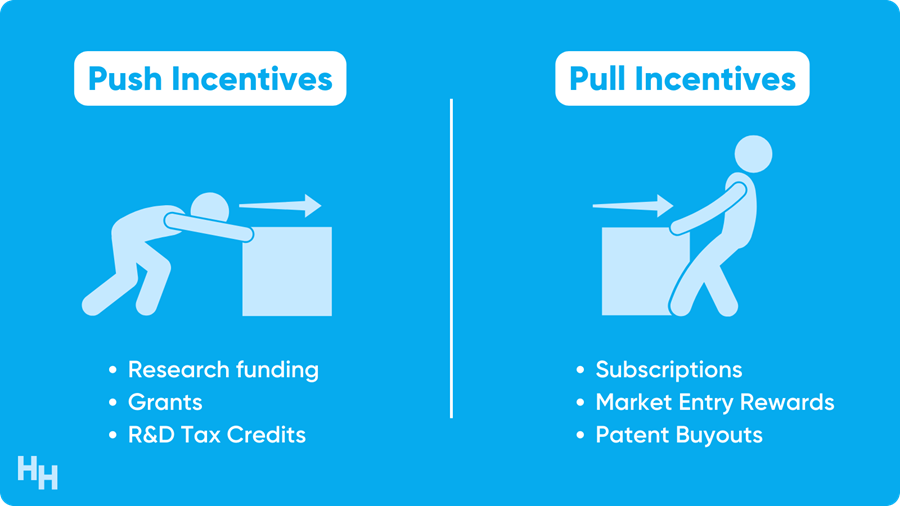
Such pull incentives may strongly incentivize companies to increase their supply of antibiotics or create novel ones. Pfizer and Shionogi’s drugs are known to treat drug-resistant bacteria infections, and we (the world) need more drugs like these. While Covid is at the top of our minds, brewing in the background is an inevitable, multi-drug resistant bacteria that can wreak havoc on society.
Why is the subscription model a good fit?
National Healthcare Spending Slows Down
National healthcare expenditures (NHE) are expected to have grown 4.2% in 2021 compared to 9.7% in 2020, a major slowdown in healthcare spending.
Decreased federal funding for programs like the Provider Relief Fund and decreased public health activity likely slowed healthcare spending in 2021. However, a rebound in patient visits as the pandemic settled likely increased private and public insurance spending.
Now, what does NHE growth look like for the rest of the decade?
Nurse Practitioner Independence in New York
New York officially granted nurse practitioners (NPs) Full Practice Authority (FPA), allowing them to provide a wide range of services without supervision. NPs in 25 states now have FPA. The FPA granted to NPs may help increase access to healthcare as the U.S. faces a formidable physician shortage.
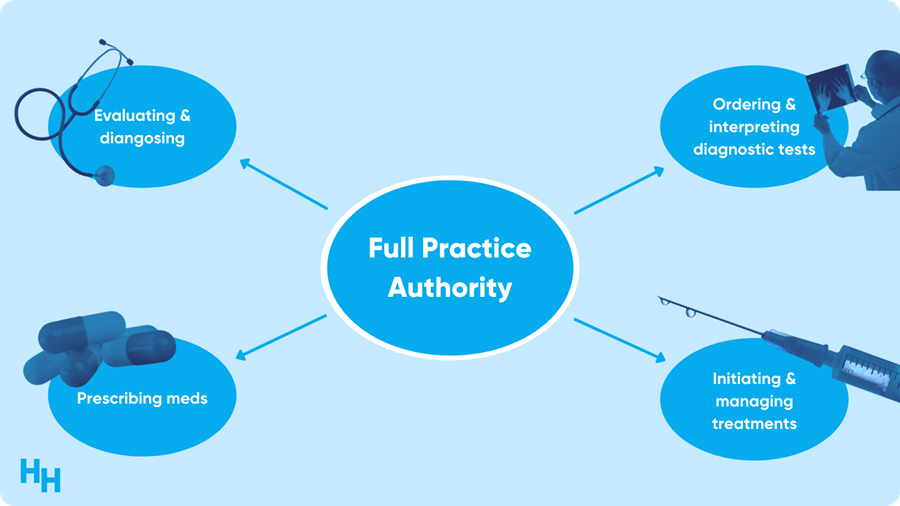
Advanced practitioners providing care at the “top of their license” is a highly contentious discussion in the medical field as health systems look for ways to cut costs. Yes, there is a shortage of physicians. Yes, NPs can take care of patients to address care gaps and do so at a lower cost than physician care.
But, are there any boundaries?
PUBLIC HEALTH
“Roe was egregiously wrong.”
The Supreme Court reaffirmed what many expected but wished would never happen: a strike down of the Roe v Wade decision.
Roe was egregiously wrong from the start. Its reasoning was exceptionally weak, and the decision has had damaging consequences. And far from bringing about a national settlement of the abortion issue, Roe and Casey have enflamed debate and deepened division. — Justice Samuel Alito
Recall that Roe v Wade established a constitutional right to abortion before fetal viability (around 23 weeks) and prevented states from banning abortion.
I will die saying this over and over again: abortion is health care. To deny access to safe and common abortion procedures before viability is unjust and neglects patient autonomy—a pillar of medical ethics.
An abortion procedure is care that is simple, extremely safe and way more common than you think. For example, around one in five pregnancies in the U.S. end in induced abortion. While you may expect abortion rates to decrease now, they won’t. People will continue to get abortions—it’s just a matter of safety. This is problematic from a health and equality standpoint.
Additionally, we’re at an interesting inflection point. On the one hand, the FDA increased access to abortion medications mifepristone and misoprostol in response to the pandemic. On the other hand, the Supreme Court voted in favor of Mississippi’s abortion law, overturning Roe v Wade and now leading to an influx of abortion restriction laws.
Here are my three general predictions:
- Telemedicine abortion will become more popular since it’s so accessible. Patients will travel across state lines, pick up mifepristone and misoprostol, drive back to their homes and carry out the medical abortion in the comfort of their homes.
- More progressive states will create “safe havens” for patients receiving abortion procedures and doctors providing them.
- The states that ban abortion will have higher maternal mortality rates than those that protect abortion by law, essentially creating a more stark divide between health care in the North and South.
Read more of my thoughts here. Check out Blake Madden‘s deep dive into how the new ruling will affect the healthcare industry here.
The Other Epidemic
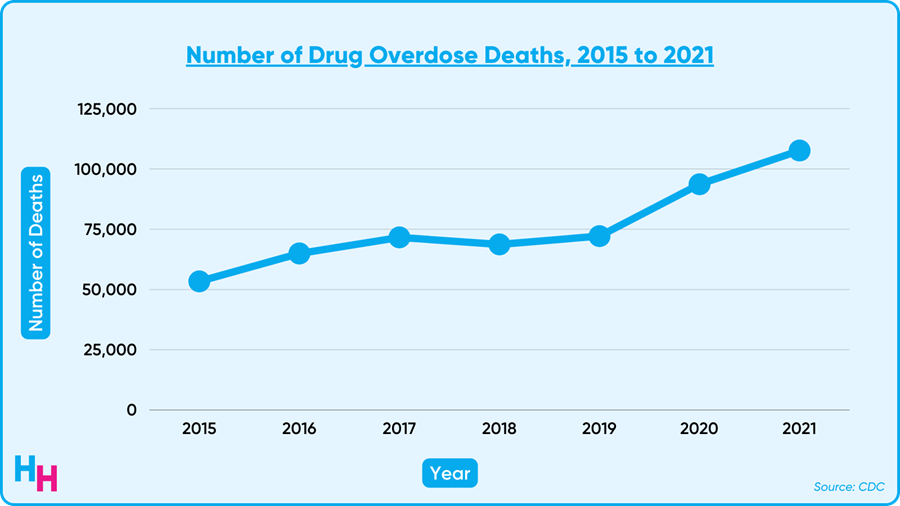
Overdose deaths have increased nearly 50% since the pandemic began, according to new data from the CDC. 2021 alone saw a record 108K overdose deaths, likely driven by fentanyl-laced drugs.
While the 108K deaths included all types of drugs, most deaths involved opioids. And of those opioid-related deaths, around 70% were synthetic opioids like fentanyl, which is up to 100x more potent than morphine. The overdose toll on individuals and society is devastating, with young people amassing greater than 1.25 million years of life lost.
How should we continue to address the opioid epidemic?
The End of the Public Health Emergency
Covid is still spreading through communities and is by no means “over.” However, sometime in July, the government will likely decide whether to extend the public health emergency (PHE). If the PHE isn’t renewed, what will the implications be? Find out here.
MEDICINE
The Future of Weight Management
The Journal published Phase III clinical trial results of Eli Lilly’s weight-loss drug, tirzepatide. These final results are a huge deal that has implications for solving the metabolic health crisis in the U.S. (and much of the world).
In this Phase III, double-blind, randomized control trial, 2,500 participants with a BMI over 30, or 27 with more than one weight-related comorbidity that’s not type 2 diabetes, were randomized to either a placebo group or three groups of varying doses of tirzepatide. At the end of the 72-week study period, participants taking tirzepatide, no matter the dose, lost significantly more body weight than those in the placebo group.
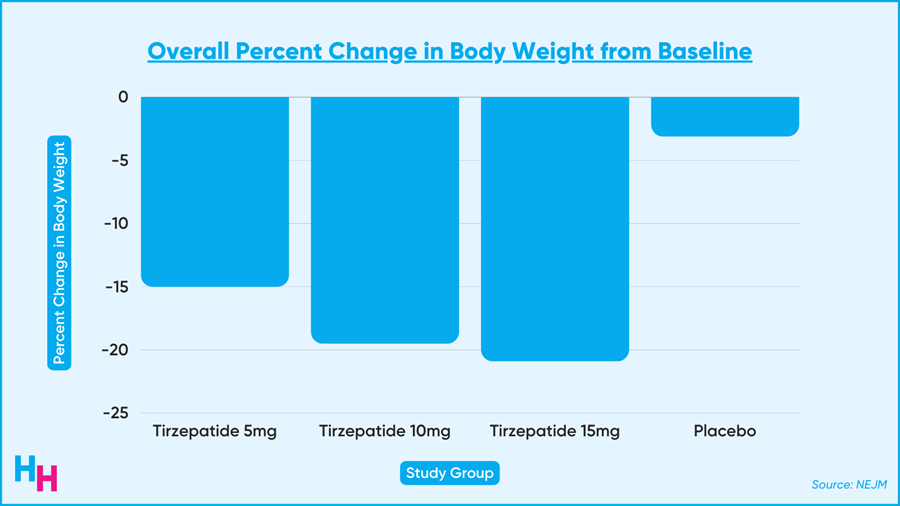
The future of weight loss management is looking bright. Read more of my thoughts here.
DIGITAL HEALTH
Digital Health’s Icarus
Digital mental health company Cerebral announced a new focus on value-based care and severe mental illness like substance use disorder.
Their pivot from bread-and-butter conditions like ADHD is not surprising, given all of Cerebral’s drama over the past couple of months. However, Cerebral is in a pretty deep hole right now, and it will take more than a ladder to get out.
Need a quick refresher on the drama?
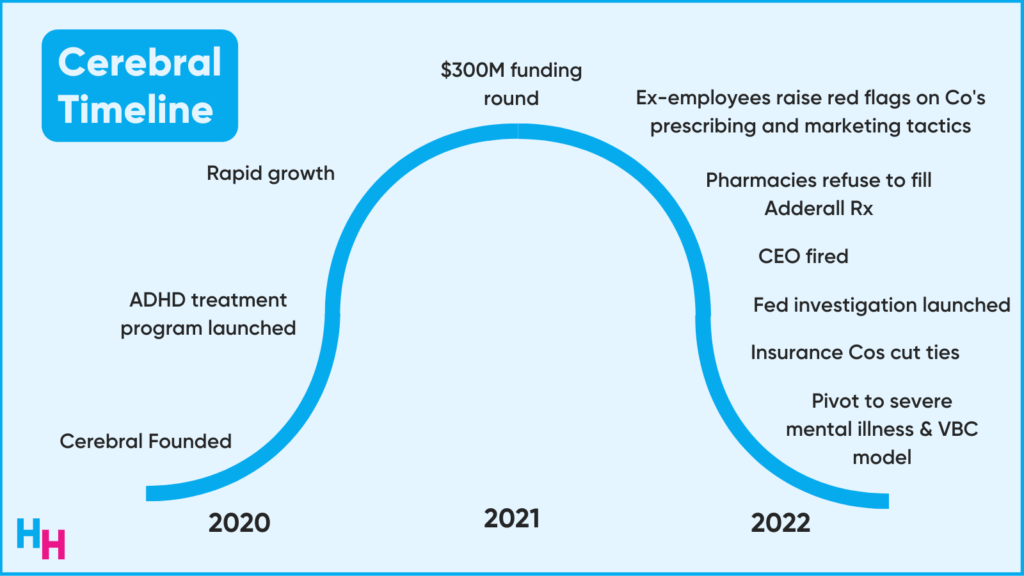
- At the beginning of the pandemic, the DEA relaxed the prescribing rules for controlled substances, allowing Cerebral to hire DEA-registered clinicians to evaluate patients for ADHD and prescribe them medication like Adderall.
- Business boomed.
- With fast revenue growth and substantial funding, Cerebral doubled down on its social media marketing to get people (Millennials and Generation Z-ers) subscribed to their platform for ADHD treatment. For example: Cerebral spent $13M on TikTok advertising from January to May this year, the third highest spender on TikTok ads behind HBO Max and Amazon.
- Employees leaked info on Cerebral’s perverse prescribing and advertising practices.
- Major pharmacies like CVS and Walgreens cut off ties with Cerebral, refusing to fill any prescriptions of controlled substances from them.
- CEO fired by the Board.
- Aetna and Optum said they’re removing Cerebral providers from their network.
What does the future look like for Cerebral?
INSURANCE
Optum Acquires LHC Group for $5.4B
UnitedHealth Group subsidiary Optum will acquire home health and hospice company LHC Group for $5.4B. The acquisition highlights a growing trend in healthcare of shifting care from the hospital to the home.
Optum is UnitedHealth Group’s health services arm, which is a behemoth of a company. LHC Group specializes in home health and hospice care, with 960 locations in 37 states. While the home health and hospice care market is quite fragmented, LHC Group makes up most of the market share at around 4.5%. The goal of the acquisition is to provide more integrated care.
LHC Group has some nice market share and revenue, sure. But what really makes them attractive to Optum is this “home health and hospice care,” an area in healthcare that’s about to take off as the population ages.
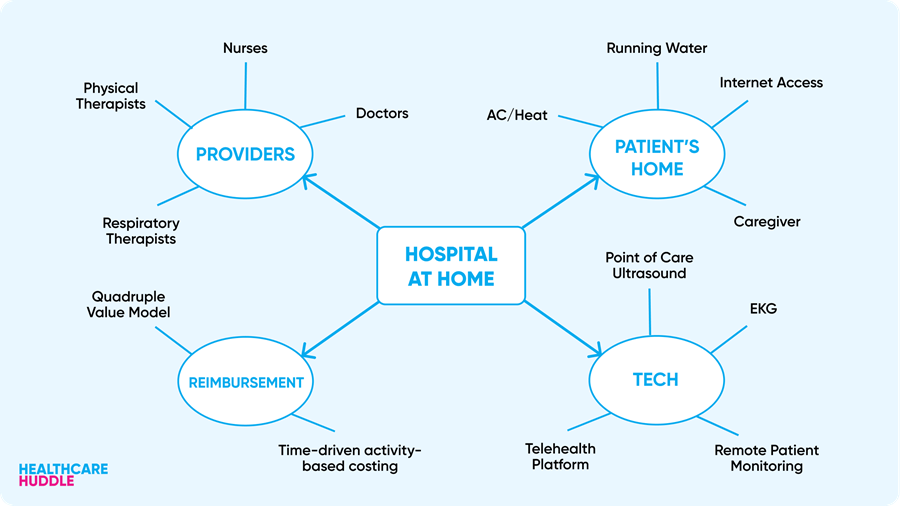
After all, the quality of home care is the same, if not better than hospital care.
Will home care be the next big thing?