21 January 2023 | Healthcare
How Health Tech is Transforming the Hospital-at-Home Experience
By workweek
The patient’s home is becoming a popular means of care delivery, no matter the acuity level. While some may think health at home is “novel,” it’s most certainly not. Forty percent of all U.S. doctor visits were performed in the patient’s home up until the 1980s. After the 1980s, however, house calls made up less than 1% of patient encounters.
So, why and how are we heading back in the direction we started?
In this article, I’ll break down the hospital-at-home movement, discuss the critical role of health tech in advancing the movement, and touch on the challenges hospital-at-home faces.
Hospital-at-Home 101
Hospital-at-home (HaH) programs provide hospital-level care in the comfort of the patient’s home instead of the hospital. It’s a pretty simple concept.
It turns out physicians can manage classic, high-acuity illnesses outside of the hospital setting, achieving the same—if not better—patient outcomes compared to the hospital setting. These classic, high-acuity illnesses include heart failure, pneumonia, cellulitis, COPD, and complicated urinary tract infections. Patients in HaH programs are stable and don’t require intense or resuscitative treatment.
There’s robust evidence suggesting HaH care is high-quality, cost-effective, and safe. A randomized control trial out of Mass General Brigham analyzed its two HaH programs compared to the inpatient setting and found the following:
- A significant 36% reduction in costs of acute care episodes for the HaH group.
- Lower 30-day readmission rates (7% vs 23%) in the HaH group.
- Fewer laboratory orders and diagnostic imaging in the HaH group compared to the inpatient group.
So, what’s the process for enrolling a patient in a HaH program?
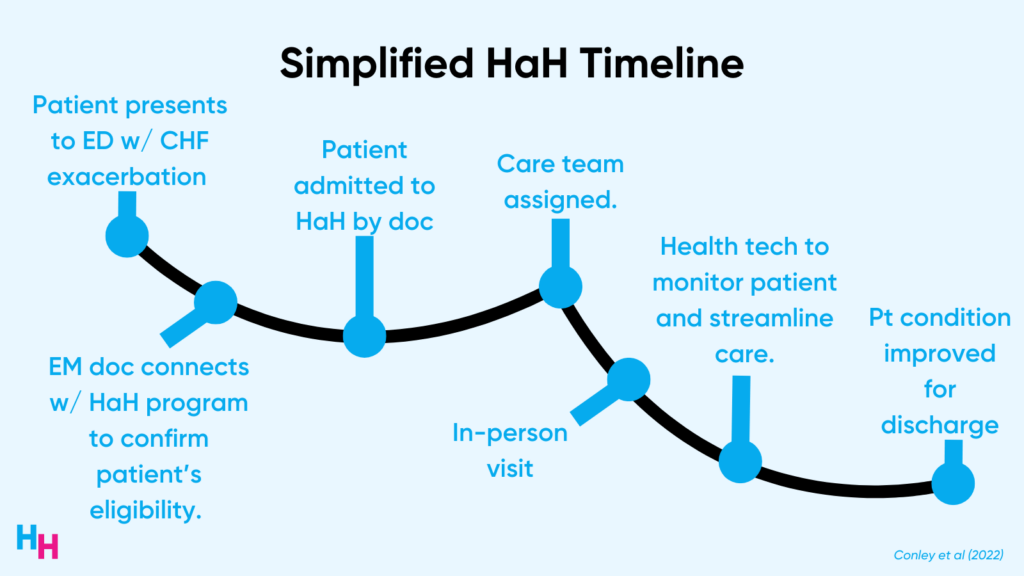
Let’s say a patient with congestive heart failure presents to the emergency department with swollen legs and difficulty breathing when lying down. The EM physician determines this is a CHF exacerbation and connects with the HaH program to confirm the patient’s eligibility in the program. The patient is admitted at home by in-person clinicians. A care team is assigned, and a plan is made utilizing health technology (telehealth, remote patient monitoring, and workflow platforms) to monitor the patient at home and streamline care. Once the CHF exacerbation is treated, the patient is discharged from HaH care.
HaH programs have picked up steam throughout the pandemic for two reasons:
- HaH reimbursement
- The advent of robust health tech
In November 2020, CMS began widely accepting Acute Hospital Care at Home waivers. This waiver removes CMS’s 24-hour on-site nursing requirement, meaning nurses in HaH programs can visit patients a couple of times per day, which is more effective. The Acute Hospital Care at Home initiative also provides diagnostic-related group (DRG) reimbursements for HaH care, essentially reimbursing home care at the same rate as inpatient care.
260 hospitals are now participating in a HaH program, compared to around two dozen pre-pandemic. While the waiver was set to expire once the public health emergency ends, congress extended the waiver until the end of 2024 in the recent Omnibus bill.
There’s No HaH without Health Tech
I said the HaH concept is “simple,” but initiating HaH care is complex and requires robust health technology. While 2022 digital health funding declined significantly compared to 2021, funding into key areas such as telehealth, remote patient monitoring, and workflow remained on top. Products and services within these key areas allow HaH programs to function effectively and scale.
Telehealth
Telehealth utilization spiked during the pandemic and has become a widely accepted means of care delivery among patients (all demographics) and providers.
Such wide acceptance has facilitated telehealth use in HaH programs, allowing for a blend of in-person and virtual visits. Typically, the physician or advanced practitioner overseeing the patient’s care will visit the patient in person for the first couple of visits. These initial in-person visits can serve to acquaint the patient with the technology being used during HaH care and allow the primary provider to gather the whole picture (living conditions, hazards, body language) of the patient, establishing rapport before handling care remotely.
Telehealth visits with the patient can happen frequently or infrequently, depending on the patient’s progress. Additionally, visiting nurses or paramedics can assist in telehealth by performing a physical exam, medication administration, physical therapy, or wound care for the provider in real time.
Preliminary data from a randomized control trial found that patient safety isn’t compromised during remote visits but may require an additional in-person visit from the leading provider in 20% of patients.
Remote Patient Monitoring
Providing hospital-level care at home requires continuous monitoring of many acutely-ill patients. While visiting nurses and paramedics may provide such monitoring for low-acuity patients, continuous remote patient monitoring (RPM) may be required for moderate- to high-acuity patients. Examples of RPM technology include the following:
- Pulse-oximetry
- Blood pressure
- Respiratory rate
- Fall monitoring
- Single-lead EKG
- Telemetry
RPM products provide alerts to the physician or advanced practitioner when the patient’s vitals change significantly or become abnormal. When an alert like this happens, the provider can engage the patient in an on-demand telehealth visit to figure out what’s going on. If needed, the provider may visit the home, send a nurse, or send a paramedic.
While RPM technology is becoming more popular, it must be rigorously tested to ensure it’s valid and reliable.
Workflow
HaH requires the same, if not more, coordination than the in-patient setting.
Think about it. In the inpatient setting, if you place a medication order in Epic, the nurse is notified and retrieves the medication to administer to the patient. This coordination must happen in the home. But there’s no drug dispensary machine 20 feet from the patient’s bed or a nurse within yelling distance at all times. So, care must be streamlined.
Robust coordination between all stakeholders and touchpoints in the HaH process is needed for HaH care to run effectively. This is why startups like Inbound Health, which is streamlining the whole HaH process, are highly valuable.
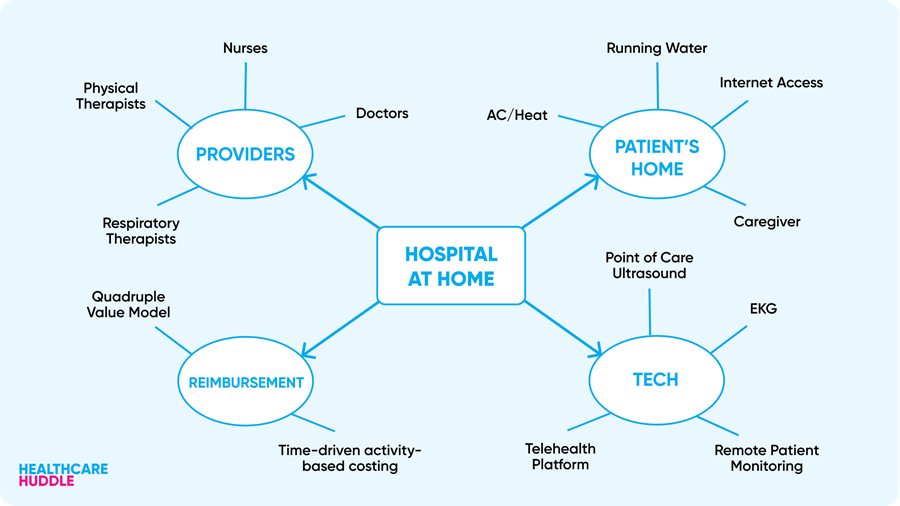
Overall, robust health technology spanning telehealth, RPM, and workflows allows for high-quality, streamlined patient care that can scale across hospitals and state lines. Without such technology, HaH would not be as effective as it is today.
Dash’s Dissection
Home healthcare spending was projected in 2018 to grow 7% annually from $103 billion to $173 billion by 2026. This was pre-pandemic, though. The pandemic has catapulted the launch and acceptance of HaH programs, likely making annual spending growth higher than originally projected.
This spending datum includes funding into health tech areas that are enabling HaH, including on-demand healthcare ($2.4 billion raised in 2022), non-clinical workflow ($2.2 billion raised in 2022), and care coordination ($1.6 billion raised in 2022). Startups to keep an eye on in this area include Inbound Health, Homeward Health, Dispatch Health, and Tytocare.
We’ll certainly see continued funding into digital health startups offering technology to enable HaH programs. In January 2022, I wrote about HaH and had the following prediction:
Lastly, where CMS goes, so do startups. I predict we’ll see current and new startups shift their focus to creating necessary tools and resources for hospitals to run robust HaH models. This can be a hot area for remote patient monitoring companies, travel nursing agencies and telehealth platforms.
A year later, it doesn’t seem like I am too far off!
Despite the hype, HaH programs and technologies aren’t perfect:
- There are many point solutions to facilitate HaH care, but these point solutions are not integrated. Therefore, the health tech used in home care is quite fragmented (as is the rest of U.S. healthcare, so this really shouldn’t surprise you).
- Health tech is inherently confusing for first-time users. When the first-time user is an acutely-ill patient, health tech becomes ineffective. So, the challenge for health tech companies is making their technology intuitive to use by minimizing friction: a 95-year-old should easily understand how to answer a telehealth call from their physician.
- HaH programs assume the patient has reliable internet access at all times no matter the location, providers can easily commute to the patient’s home (which is easier in urban areas as opposed to rural areas), and a caregiver is available to care for the patient when assistance isn’t there. Such assumptions may not always be valid. Therefore, HaH programs may perpetuate health inequities.
Lastly, there’s immense value in visiting a patient’s home to deliver care. At my institution, we’re required to do home visits during our clerkship in geriatrics. It was eye-opening. I saw a patient’s wall full of family photos, how they organized (or didn’t organize) their medications, what food they had in their pantry, and how hard it was to walk up four flights of stairs to get to their apartment. I talked to Dr. Daniel Arteaga about this. He frequently sees patients in their homes and learns so much about his patients, allowing him to better care for them than he would in the hospital setting.
In summary, HaH programs function to deliver acute-level care in the comfort of the patient’s home instead of the hospital. HaH became immensely popular throughout the pandemic thanks to reimbursement opportunities and the advent of robust health tech. The HaH movement will grow quickly from here as value-based reimbursement models become mainstream and health tech advances. I predict HaH care, especially in urban areas, will make up 25% of all hospitalizations by the end of the decade.
HOME HEALTH
- CVS Buys into Home Health Company Signify Health for $8 billion (link)
- Optum Acquires LHC Group for $5.4 billion (link)
- MyMichigan Health Announces Launch of Hospital at Home Program (link)
If you enjoyed this deep dive, share it with colleagues. Sign up for the Healthcare Huddle newsletter here.