27 June 2022 | Healthcare
Unwarranted Clinical Variation
By workweek
Same age. Same sex. Same illness. Different treatment. This is unwarranted clinical variation; it’s care that’s not consistent with a patient’s preference or related to a patient’s underlying illness.
The U.S. has a significant problem with unwarranted clinical variation, stemming from its inherent complexity. This isn’t a benign problem, though. The sequelae of such variation include low-quality care and increased costs of care delivery.
The Deets
Unwarranted clinical variation is nothing new in healthcare. A researcher in the U.K. was the first to report on clinical variation in the 1930s showing local differences in rates of tonsillectomy among British school children. Since then, clinical variation has only become more prominent in the United States
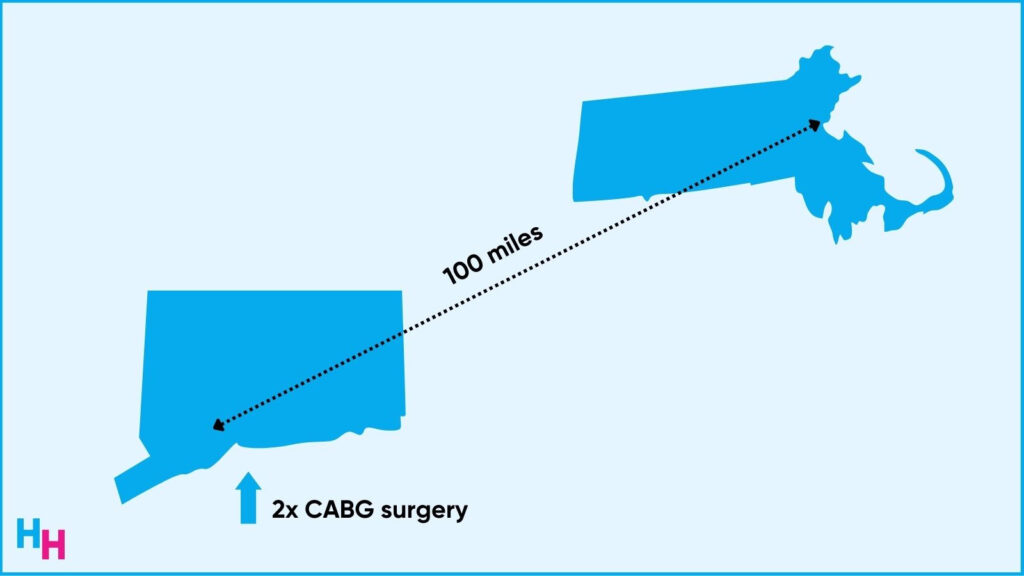
For example, in the 1980s, researchers found that those living in New Haven, Connecticut, were twice as likely to receive coronary artery bypass surgery than their matched counterparts in Boston, Massachusetts. The type of care residents received in these two cities—just 100 miles away from each other—was neither consistent with clinical evidence nor patient’s preference, background or underlying illness.
Despite 40 years of medical advancement, variation still proliferates throughout the healthcare system and not just between geographies, but within them, too. A recent JAMA article highlighted physician practice variations in common clinical scenarios (coronary artery disease, diabetes care, COPD care, etc) within five U.S. cities. The study found appreciable practice pattern variations across all the clinical scenarios, despite clear guidelines indicating what the care should be.
Why, Though ?
I’ve found that unwarranted clinical variation stems from two problems:
- The increasingly complex healthcare system.
- The exponential growth of medical knowledge.
Fifty years ago, doctors had a manageable number of medications to choose from when treating a patient. Now, doctors have nearly 10,000 drugs to choose from in addition to the 300,000 over-the-counter products. To decide which medications to prescribe and recommend, doctors may also choose to order a diagnostic test such as an MRI, CT scan, stress test, you name it. Novel diagnostic tools appear more frequently with increasing accessibility, adding to the system’s overall complexity.
Along the same lines, we wouldn’t have seen such growth in technology without the exponential growth of medical knowledge. The exponential growth in medical knowledge makes it impossible for doctors to stay current on the latest and greatest information and technology. It’s estimated that a doctor would need to read twenty articles a day, 365 days a year, to keep up to date with the literature—and this study was performed in the ’90s!
So, how do physicians address the increasingly complex healthcare system and the exponential growth of medical knowledge? By primarily relying on their clinical expertise. Where do they gain their clinical expertise? During residency and fellowship.
Where physicians train will largely dictate how they practice medicine throughout their clinical career. But even the type of training varies between regions. Think about it. A resident who trains in a rural hospital and then works in an urban setting will approach patients differently regarding diagnostics and treatments. The same is for an urban-trained resident (with specialty consultations available whenever) who then works in a rural area (limited specialty consultations).
The Impact
Unwarranted clinical variation in our health care system suggests that individuals may not be receiving the best care or that healthcare resources are being misused.
The Dartmouth Atlas of Health Care (a fabulous resource) analyzes the healthcare system to understand its efficiency and effectiveness. For example, the Atlas reports in some U.S. regions, less than 45% of Medicare patients were appropriately vaccinated, while in others, the figure was over 95%. The Atlas also indicates that 30%–40% of patients in America do not receive care consistent with the current evidence and that 20%–25% of care provided is unnecessary or potentially harmful.
Additionally, over-utilization of supplies accounts for most of the two-fold regional variation in total per capita spending on patients aged 65 and above. For example, a New England Healthcare Institute report found that the variation costs between high and low utilizing regions approach 30% of total healthcare spending.
The Solution
A growing and popular method to tackle unwarranted clinical variation is using Clinical Decision Support systems (CDS). A CDS system is a computer program to help health care professionals make clinical decisions.
By fostering collaboration, reducing medical errors and notifying providers of pertinent medical information, CDS systems can maintain a high quality of care while reducing costs. CDS systems are designed to sift through massive amounts of digital data to help providers decide on treatment steps, alert the physician of any errors (e.g., dangerous medication interactions), streamline workflow and improve communication between staff.
A Kauffman Hall survey reported that 56% of hospital organizations make effective use of CDS systems, suggesting a growing desire of organizations to reduce unwarranted clinical variation. At the Mayo Clinic, for example, hospital staff took advantage of CDS systems to minimize the variation experienced in nurse triage.
Mayo Clinic’s CDS systems were used during flu season (pre-Covid-19) when nurses received 5,600 calls a month. The CDS system automatically updated nurses with the most recent community flu data along with notes to inform the nurses what data and steps have changed regarding flu management (note: it’s usually supportive care, which can be done at home).
The nurses reported that about 1,500 callers initially intended to stay home for their care, and with the use of CDS systems, the nurses helped redirect an additional 3,250 patients to stay home. These 3,250 patients could self-care at home instead of wasting resources to see the doctor, which would have resulted in the same outcome.
However, despite all the potential benefits of CDS systems, their widespread success has been variable because of the challenges they face, such as loss of physician autonomy, alert fatigue and poor adoption.
Food for Thought
There’s a general consensus among providers to reduce unwarranted clinical variation. But, don’t mistake this to mean we should reduce all types of clinical variation.
The truth is that one size may fit most but rarely fits all.
Said another way, necessary variation can improve patient care. For example, say you’re a primary care provider and a patient with depression comes to you requesting medical treatment for their depression. First-line therapy is usually an SSRI such as paroxetine. But, the patient also adds they want to quit smoking. The necessary variation, in this case, may be to prescribe bupropion, which can treat depression and help with tobacco cessation.
Final Thought
Unwarranted clinical variation is a pervasive problem in healthcare, leading to increased healthcare spending and poor healthcare outcomes. Technology like clinical decision support systems can help combat such unwarranted variation.
But, sometimes variation is necessary.
As medicine and startups continue to emphasize what the patient wants, it’ll be important for physicians to find the balance between necessary and unnecessary clinical variation.