Good morning, Hospitalogists!
Today, we’re diving into the world of provider credentialing. I had a ton of fun learning about this major pain point alongside Medallion, so I’ve teamed up with them to talk about the problems Medallion is solving in the space.
I hope you enjoy learning about a company and service that has proven to alleviate major headaches while providing clear ROI to its clients – a rarity in much of digital health!
This essay is a sponsored post in partnership with Medallion. I write these posts for companies with products or missions I believe can provide value-adds for Hospitalogy subscribers, many of whom work with/for hospitals or provider organizations that deal with issues like credentialing on a daily basis. If you’re interested in a sponsored deep dive, please reach out to [email protected]!
Talking Provider Credentialing with Medallion
What you need to know:
- Medallion does credentialing faster with better quality. They do the little things right, automate what they can, and get providers in-network faster.
- Quicker credentialing = faster reimbursement. Medallion’s credentialing service provides clear financial ROI for healthcare organizations, including better revenue cycle management and stronger relationships with payors.
- Credentialing in its current state is terrible. It’s intricate and labor-intensive.
- Payors like to take their sweet time with these types of things, which makes a bad credentialing process worse.
- Doing credentialing the wrong way creates compliance, scalability, and cash flow issues.
- Medallion is a tech-forward credentials verification organization (CVO).
- You can schedule time or a demo with Medallion here.
The Healthcare Theme of 2024: Doing more with Less.
Resource capacity is top of mind for healthcare executives nationwide. Amid layoffs and a tough operating environment entering 2024, hospitals, physician practices, and everyone in between are having to find ways to stretch their existing personnel.
Along with labor struggles, for provider organizations not named HCA, payors aren’t budging on reimbursement despite the acute issues facing providers.
We’re between a rock and a hard place here, fam. So, where do we go from here?
Based on convos I’ve had with operators and consultants in the space, almost all are actively looking to find ways to cut costs and optimize operating efficiencies within their organizations.
How does that take shape? Apart from the obvious headcount reduction, care delivery organizations are taking a harder look than ever at vendors that can provide clear cost savings or outsource key functions to free up existing administrative or clinical personnel.
For instance, we’ve seen health systems offload a boatload of IT services and thousands of FTEs to Optum. Providers and hospitals are outsourcing revenue cycle management services to firms that promise to boost cash collections and drive better cash flow. On a more operational front, we saw HCA partner with Augmedix to pilot its AI scribe / ambient documentation solution in its ERs to free up clinician time and boost productivity.
What’s the common link here? All of these services provide (or at the very least, promise to provide) their customers with clear financial returns – or operating efficiencies that can easily be attributed to financial returns in some way – in exchange for using and paying for that vendor’s services.
Today, I want to introduce you to a firm that does this exact same thing with the credentialing process: Medallion.
Medallion Solves the Complexity of Credentialing.
Provider credentialing is a much-needed but stupid-complicated process in healthcare. At a high level, the credentialing process involves a bunch of steps to get a clinician in-network with a payor.
It’s an utterly thorough process that verifies a healthcare provider’s qualifications and history to get in-network status with Medicare, Medicaid, & commercial payors.
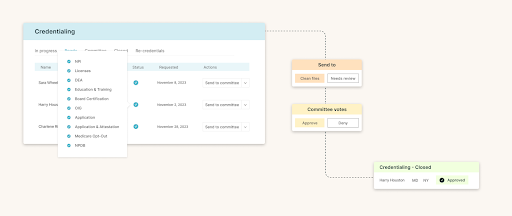
Those steps include things like application receipt, review, data verification, committee evaluations, to approvals, and plenty of other small things that can trip up even the most organized person.
Join the thousands of healthcare professionals who read Hospitalogy
Subscribe to get expert analysis on healthcare M&A, strategy, finance, and markets.
No spam. Unsubscribe any time.
And don’t forget organizations are required to repeat this and verify credentials every 2-3 years. With every contracted payor.
As a provider organization or revenue cycle management company, doing credentialing in-house on your own sucks.
The process, like many other administrative tasks in healthcare, requires too many man hours, causes frustration, and results in compliance issues if your team misses something.
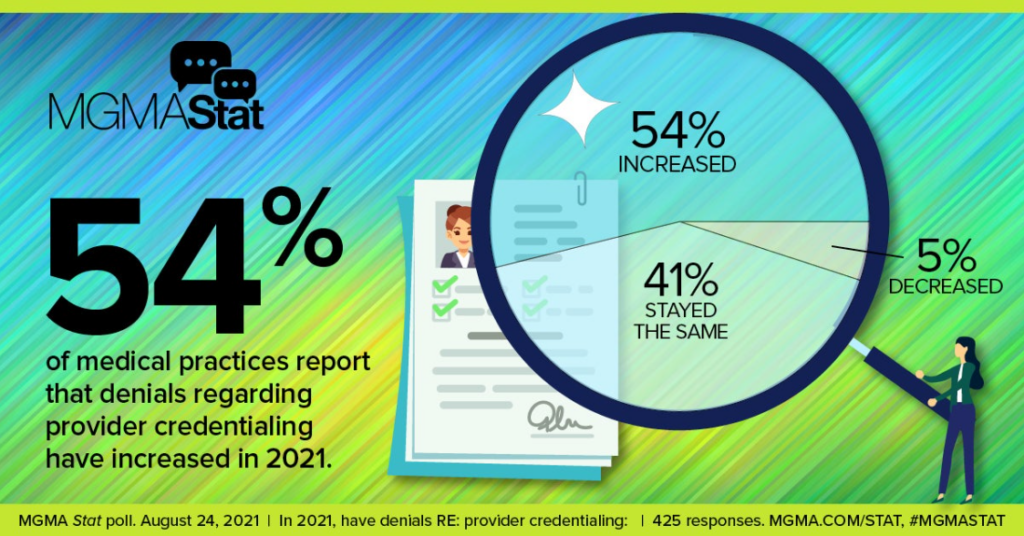
Every private and public payor has its own idiosyncratic credentialing process. Most take 90-120 days to respond to a request, but sometimes unwinding their backlogs can take months.
Ultimately, these issues cause cash flow problems for organizations time and time again. Delays getting paid. Denials. Problems verifying physicians with insurers, creating an accounts receivable backlog. Net revenue/collections ratios plummet. Bad debt accruals skyrocket.
Given time constraints, a problem in credentialing kills an organization’s ability to scale.
Sound familiar?
Medallion identified these common pain points as a clear ‘jobs to be done’ solution in healthcare.
So they built a better credentialing platform.
How Medallion Solves the Credentialing Problem.
A common theme in healthcare is the need to reduce vast administrative costs and complexity, and burnout. Medallion couldn’t agree more and has built a credentialing platform to echo those beliefs.
To that end, Medallion offers providers an NCQA-certified CVO solution that enables healthcare organizations to move faster and get ahead:
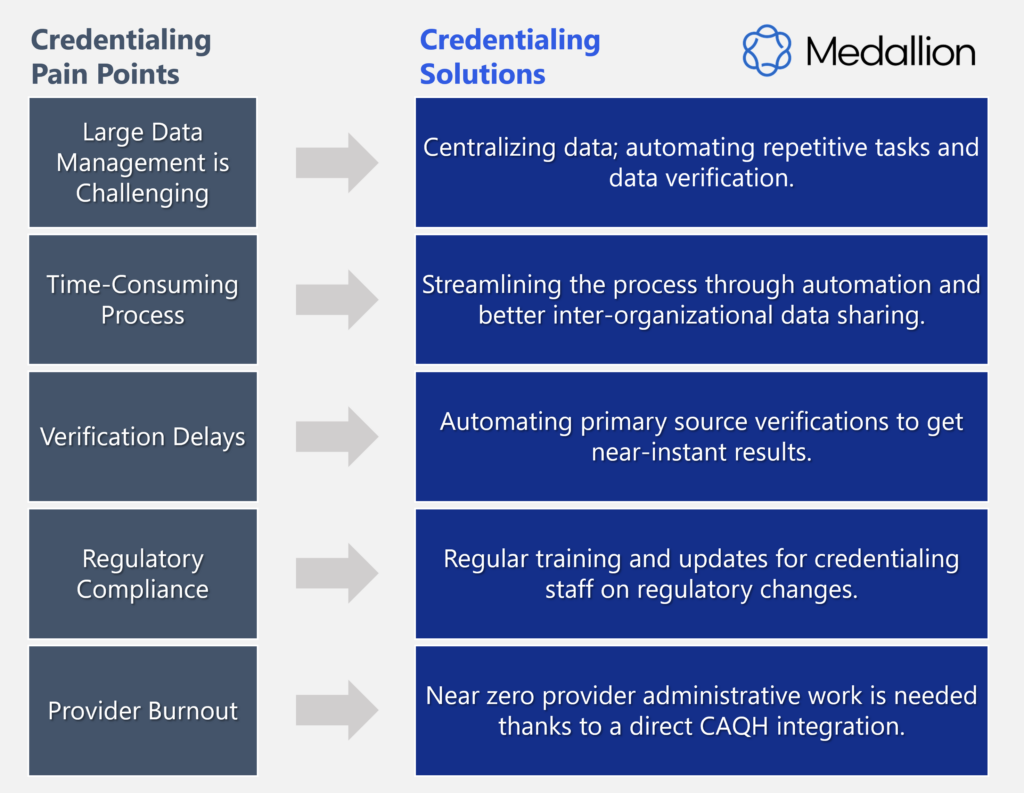
A single, faster platform: Medallion operates a dynamic credentialing platform. It hosts pre-built integrations to hundreds of primary sources, allowing organizations to automate primary source verification and speed up credentialing. Having a one-stop shop for all things credentialing simplifies tasks for central business offices and administrative personnel.
Don’t reinvent the wheel: Medallion has already done the blocking and tackling for provider groups and iterates its process to continually improve its solution and automate the little things wherever possible. For instance – Medallion’s solution puts the following ‘in-between’ functions on auto-pilot such as:
- Auto-checking state licenses and board certifications.
- Investigating sanctions to ensure disqualified providers are out of networks.
- Sending automated alerts about important provider eligibility changes, helping you manage compliance and stay within regulations.
Medallion is built for scalability: The platform’s capability to have 40,000+ providers and handle over 91,000 licenses, enrollments, and credentials highlights its robustness. As healthcare entities expand or diversify, Medallion effortlessly scales up to accommodate growing needs.
- Every payor – public and private – has its own credentialing process. Medallion already has these nailed down.
- Physician practice management companies, telehealth firms, and everyone in between expand more effectively using a credentialing service like Medallion’s.
Delegated credentialing is a game changer: Simply put, delegated credentialing involves payors shifting the responsibility of provider credentialing to trusted, credible providers with whom they have an established relationship. It’s a faster path to credentialing and one that Medallion has leveraged for its clients to get clinicians credentialed faster. Payors are increasingly adopting delegated credentialing to speed up the process for preferred provider groups. Bigger picture: as new pathways to credentialing like delegation emerge, Medallion will stay at the forefront of these alternatives.
Medallion: Credentialing simplified.
To summarize, Medallion simplifies and improves a critical bottleneck and common pain point in healthcare. By streamlining and speeding up credentialing, healthcare professionals can prioritize patient care, drive the bottom line, and scale their operations faster with fewer headaches.
For provider groups, digital health companies, and all stakeholders, partnering with Medallion is not only an option but a necessary move in today’s healthcare industry.
Even if you don’t ultimately use Medallion, it’s worth having a conversation with them to make sure you’re not missing something in your own credentialing process.
Links and Resources:
- Schedule a demo
- Elevating payer-provider collaboration with streamlined enrollment and credentialing solutions
- Payer enrollment vs. credentialing: what’s the difference?
- More about Medallion’s credentialing solution
- How to establish delegated agreements for efficient enrollments
- How to enhance revenue cycle management with effective provider credentialing
- What is delegated credentialing and how to use it to get more control over revenue cycles

