Happy Thursday, Hospitalogists!
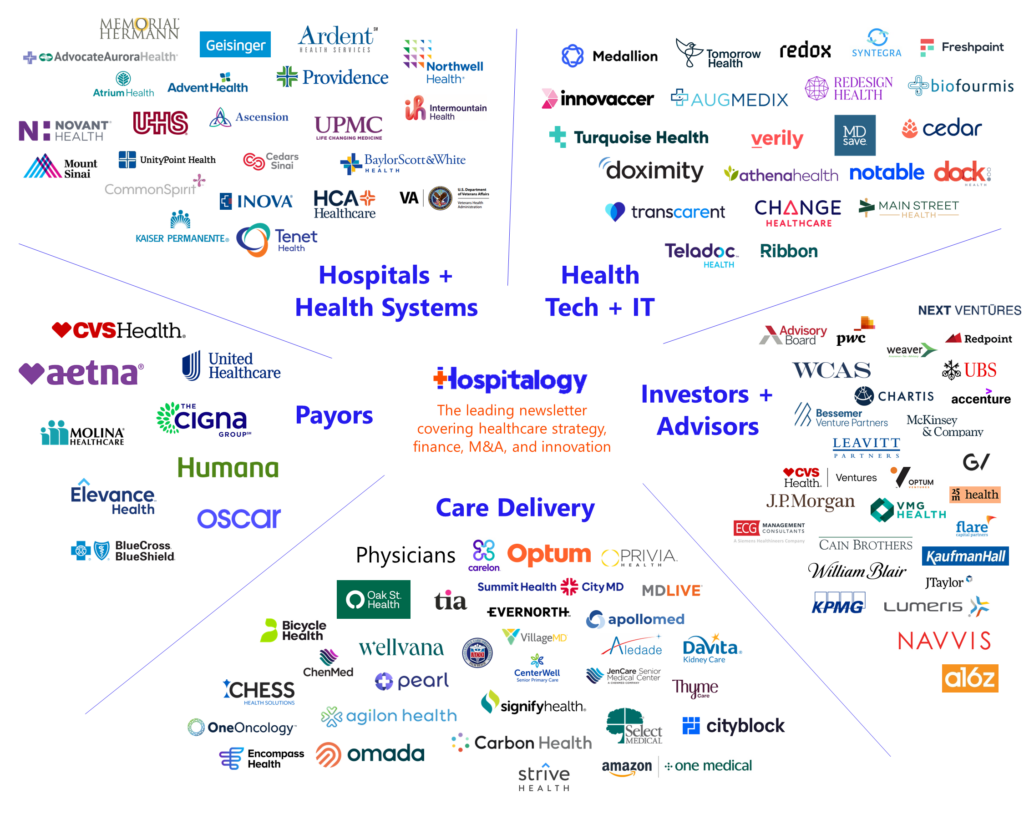
The Hospitalogy Guest Posting series continues today with a great write-up on the current state of AI in healthcare – an overview of the space, dynamics at play, and real-world use cases with firms tackling those issues.
I’m excited to bring you this piece from the collective minds of Eric Thrailkill, Chairman at Project Healthcare; Dr. Adam Silverman, Chief Medical Officer at Syllable; and Lauren Hatcher, M.D. and M.B.A candidate at Vanderbilt. Give them a follow on LinkedIn. I am grateful to each of them for putting serious time and effort into this piece and hope you guys enjoy it.
As always, if you have any thoughts about the piece, please respond to the e-mail and I’ll pass them along to the authors!
Thanks so much to Augmedix for sponsoring today’s Hospitalogy. You guys already know how I feel about them. Check out their latest product launch, Augmedix Go.
Let’s dive in.
SPONSORED BY AUGMEDIX

If you’re in healthcare, you know the tedious pain of medical documentation.
It’s time-consuming, error-prone, and a major contributor to burnout.
Enter Augmedix Go.
A clinician-controlled mobile app, the fully automated Augmedix Go uses automatic speech recognition and natural language processing to draft medical notes in seconds.
These medical notes are available in real-time, allowing clinicians in acute and ambulatory care settings to promptly review the draft note and upload to the EHR.
Want to improve clinician efficiency and revolutionize your health system’s operations?
AI in Healthcare – Will We Lead or Will We Lag?
Hospitalogy Family – we’re elated to bring to you this guest column today. We hope you enjoy this piece by Eric Thrailkill, Adam Silverman, MD, and Lauren Hatcher and look forward to your comments. Don’t worry – Blake will be back in December! Now, for some introductions:
Eric: Four decades of healthcare experience, education in accounting, a CPA, and at one time – in the CIO seat of three separate national provider organizations – multi-specialty medical clinics, correctional health services, and ambulatory surgery centers. Now I’m spending time leading Project Healthcare, a program of the Nashville Entrepreneur Center, surrounded by digital health venture investing through two venture capital funds, and providing a dose of advisory (“seasoned executive”) services. From on-premise to cloud, from paper-based to electronic health records, from siloed data to warehouses.
I’m joined by two industry colleagues I truly admire, professionally and personally – Dr. Adam Silverman and Lauren Hatcher.
Join the thousands of healthcare professionals who read Hospitalogy
Subscribe to get expert analysis on healthcare M&A, strategy, finance, and markets.
No spam. Unsubscribe any time.
Adam: My thirty year career as an Internist has shown me one thing again and again. We spend a lot of money on healthcare, our outcomes aren’t good, and we hurt too many people. Many have tried to break this cycle, and many have failed. The allure of the status quo was and is too powerful. My experiences over my career have transformed a once idealistic medical student into a cynical practitioner and now a radically pragmatic entrepreneur who realizes that change (innovation) in healthcare is harder than it should be. I mean, at the end of the day we will all be patients. Why can’t we act in our own self interest to create a system we want to utilize? So to scratch this itch to do better, I joined a startup with an idea to use AI to improve access to care.
Lauren: Currently an M.D./M.B.A. student graduating in May of 2024. This clinical background and business education have given me unique insight into the broken system of clinical practice, the difficulties faced by patients, and the incentives (or lack thereof) to change the system. If my training has taught me one thing, it’s that there is a large gap between the front-line workers and the business of healthcare.
As far as AI goes, I’m fortunate to have one foot in the “real world” of medicine – the hospital wards that are by and large not implementing this technology yet – and the “hype world” of industry where everyone is talking about it. I’m also applying to diagnostic radiology residency programs where the technology is sure to have an impact. And no, I’m not worried that my future job will be replaced by AI.
The Time is Right for A.I. in Healthcare
Eric: We’ve known for some time that factors associated with longevity and quality of life are only somewhat dependent (20%) on where you receive your medical care and more likely dependent upon socioeconomic, environment, and health behavior issues. We’re also beginning to understand the “omics” impact on diagnostic and treatment responses.
What we’re missing is how to utilize all this data to actually impact patient care.
What if we had low cost, almost unlimited computational and data storage capabilities, and a seamless way of combining large data sets and leveraging cloud capabilities, to improve the administration, diagnosis, and treatment activities in the industry?
What if the information utilized by clinicians was personalized to the individual, combined with privacy, security, and appropriate data sharing agreements to power discovery well into the next decade?
And, what if the industry had the financial incentives to promote health, prevent illness, and treat disease?
Well, we do…..this witch’s brew of financial incentives, external datasets, nearly unlimited computational resources, and macro industry challenges has allowed AI to grab all the headlines…..but the tools that utilize AI to improve health outcomes and elevate the healthcare delivery experience will come in many flavors.
When We Say “AI”, What Do We Mean?
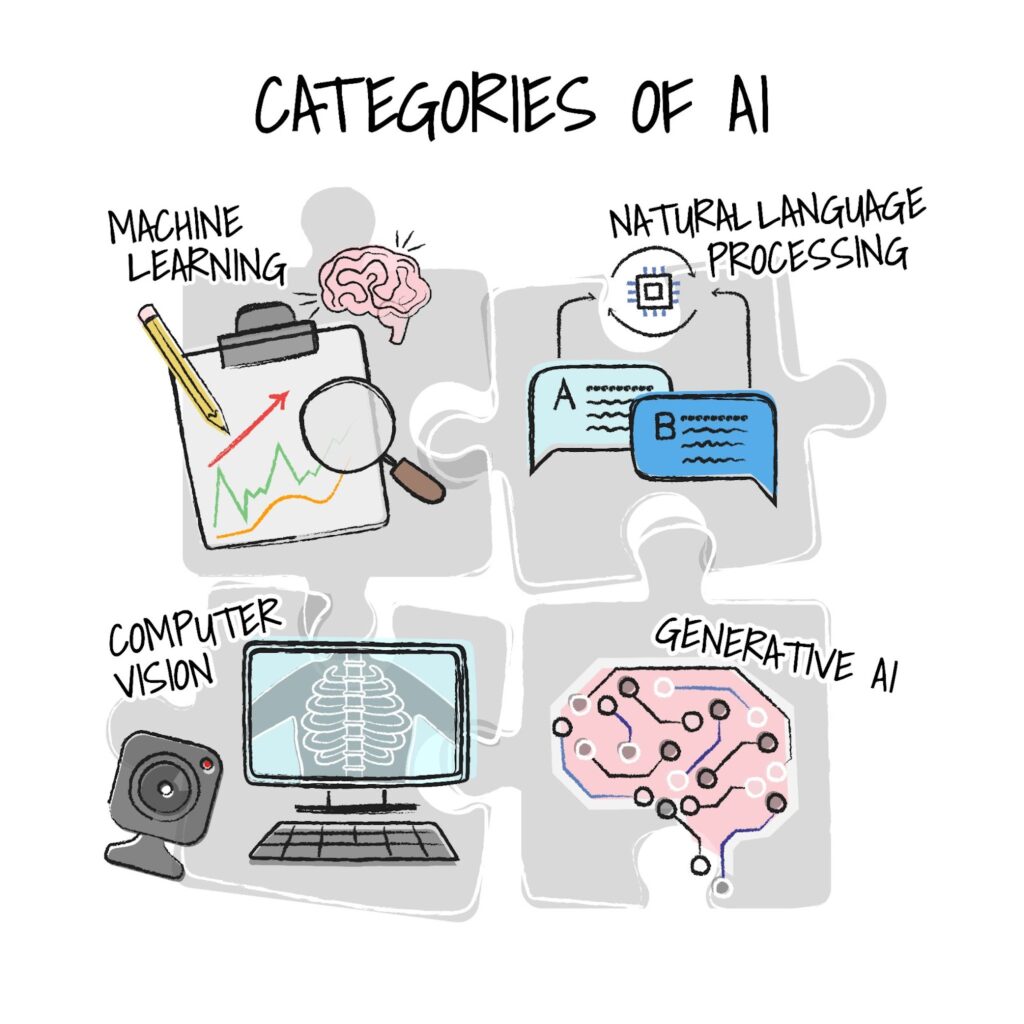
Eric: Within the realm of AI in healthcare, there are four prominent categories that hold immense potential:
- Machine Learning and Predictive Analytics (ML/Predictive) enable healthcare organizations to harness the power of data to predict patient outcomes, optimize resource allocation, and enhance clinical decision-making.
- Natural Language Processing (NLP) focuses on understanding, interpreting, and generating human language. NLP enables computers to comprehend and process text and speech and can be used to extract valuable insights from clinical notes and patient records.
- Computer Vision extends AI’s reach into image analysis and interpretation, offering applications such as radiology image analysis, pathology diagnostics, virtual nursing, and fall risk reduction.
- Generative AI opens doors to creative problem-solving, assisting clinicians with medical summaries, and creating conversational tools for patients’ communications by leveraging large language models specifically trained for healthcare use cases.
The Necessary Ingredients
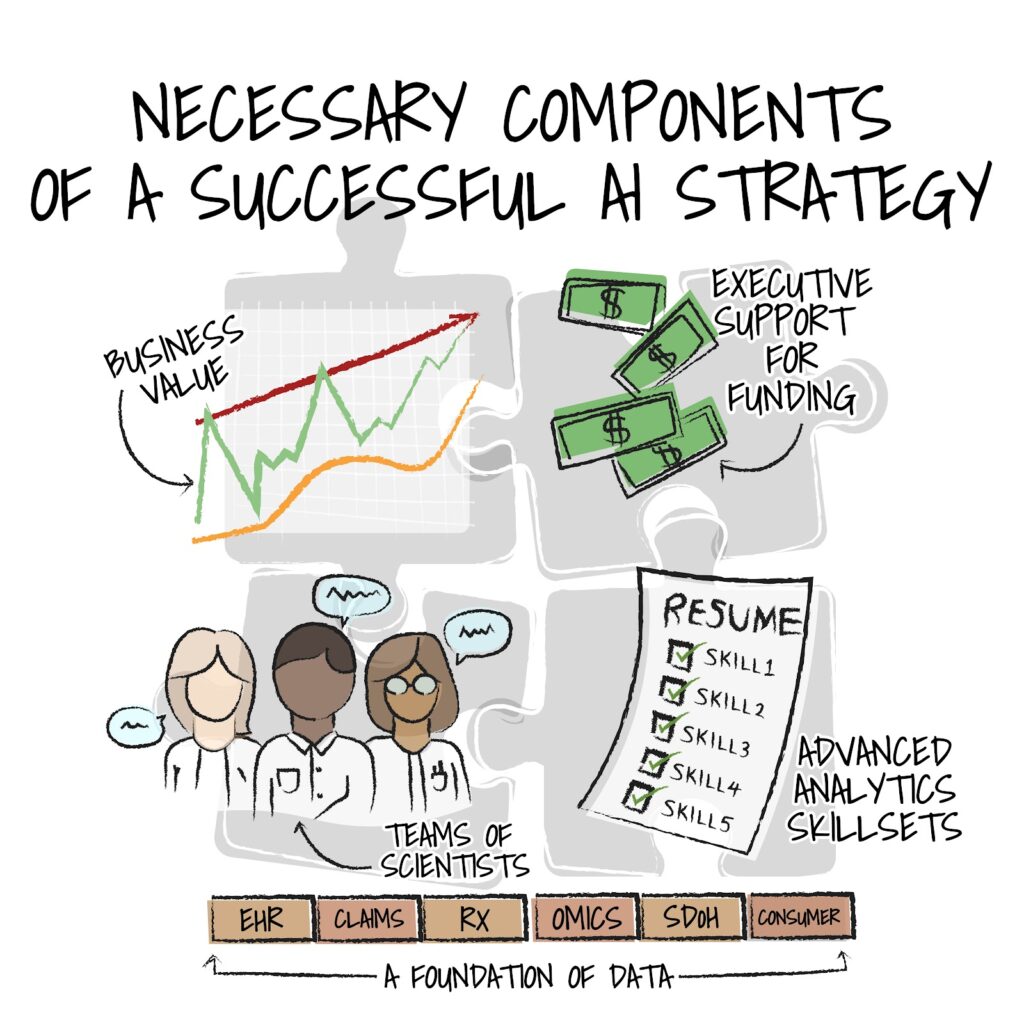
Eric: Achieving success with any of these technologies requires a thoughtful approach, because in the intricate world of healthcare, where precision and performance can mean the difference between life and death, the adoption of AI is akin to crafting the perfect culinary masterpiece.
To achieve the desired outcomes of enhanced quality, improved patient and consumer communications, and the reduction of clinician burden, hospitals and health systems must gather the necessary ingredients for this transformative recipe.
Electronic health records, genomics data, insights from social and community-based sources, claims data, operational, and financial data provide the essential raw materials.
However, data alone is insufficient; it’s the equivalent of a chef having the finest ingredients but lacking culinary expertise. To harness the full potential of AI, a skilled team of advanced analytics and data scientists is crucial.
In this recipe for success, an executive team willing to invest in the future despite the headwinds of today is the key secret ingredient. Much like a restaurant owner who continually upgrades their kitchen equipment, healthcare leaders must be forward-thinking and committed to funding AI initiatives, recognizing that the long-term benefits far outweigh the initial costs. It is quite challenging to plan for financial rewards based on superior health outcomes versus the transactional (fee-for-service) reimbursement methodologies in place today.
With data, a team of analytics experts, and a forward-thinking executive office, AI becomes a valuable ally, enabling providers to practice at the top of their license, improving patient care, and ultimately transforming healthcare as we know it.
As an example, at the recent HLTH Conference in Las Vegas (October 8-11, 2023), Roberta Schwartz of Houston Methodist Hospital and Nassib Chamoun of Health Data Analytics Institute, presented on these components and discussed how their health system was leveraging ML, predictive analytics, generative AI, and cloud computing infrastructure to interpret clinical notes in real-time, making it possible to use historical data to predict patient risk profiles (Deploying Clinical AI at Scale, Moon Stage, October 9, 2023).
An Absence of Uptake
Lauren: Although everyone is talking about it, few are actually doing it. Medical school has allowed me to rotate in virtually every field of medicine, and I’ve yet to see one provider use AI in practice. In fact, only 14% of healthcare professionals say they are currently using AI to diagnose, treat, or communicate with patients. Moreover, only 6% of health system executives have an established generative AI strategy. The reality is that medical students like me are still faxing records and uploading radiology images on CD discs from outside hospitals. With all the available technology Eric described, the glaring question is: why is utilization so low?
Perhaps the answer is rooted in the fact that healthcare business models, particularly for mature entities, become increasingly interdependent and resistant to change, especially in successful organizations. Ann Somers Hogg of the Christensen Institute researched this interconnectedness of value proposition, resources, processes, and profit formula in What are Business Models and How Do They Work in Health Care. She states, “business models determine an organization or company’s capabilities (what it can and can’t do) and its priorities (what it must accomplish). This, in turn, defines which innovations it can and will pursue.”
The resulting manifestation (low AI utilization) is contained in these four primary symptoms:
- We lack AI standards for healthcare utilization. The majority of AI and ML systems have not gone through FDA review. Of the algorithms that have gone through FDA review, the majority have received 510(k) clearance, which usually does not require randomized controlled trials to show safety and efficacy. However, this may be changing – Non-governmental organizations like the Coalition for Health AI (CHAI) and the Peterson Center on Healthcare are tackling these complex issues, and on October 30, 2023, President Biden delivered an Executive Order on AI.
- Many physicians and patients are resistant to the technology. Approximately one third of healthcare professionals think that the use of AI in healthcare will hurt more than it helps, and 60% of surveyed Americans are uncomfortable with their healthcare provider relying on AI to diagnose their disease or recommend treatment.
- Data in healthcare is siloed, and the training of models is a challenge. To guard patient privacy, hospitals protect data needed to build AI models. Even if enough data is obtained, additional data is needed to validate the model on new populations not included in the original data set. Additionally, in clinical scenarios, findings and diagnoses are frequently interpreted and not absolute, and even agreement among experts can be difficult to achieve. Finally, clinical context can be important, so extracting data from the EHR is another necessary step. All of this makes training the AI based on labels complex.
- Existing reimbursement models do not prioritize investment in AI. To quote Dr. Lily Peng on the NEJM AI Podcast, “The way we pay for healthcare changes the way technology gets implemented.” Currently, the biggest barrier to AI implementation according to health executives is resource constraints. Overcoming the upfront costs will only be possible if and when health systems engage in value based care contracts. These contracts incentivize care coordination, interoperability, and workflow optimization, all of which are capable with AI.
Despite these challenges, medicine is changing with a new generation of physicians (myself included) entering the field, with some even getting degrees in AI. We are comfortable with technology, eager to implement it in a way that benefits our patients, and excited to relieve the administrative burden that currently contributes to burnout. In addition, there are a convergence of factors at the system level that are making it possible for healthcare to lead when it comes to AI.
Additional Barriers to Overcome
Adam: Lauren is absolutely correct in looking at the macro level reasons for lack of adoption, but there are also a host of cultural barriers within the health system sphere of operations that must change. Here are just a few:
- Health systems are not monolithic organizations with streamlined leadership and decision making infrastructure. They are more like a confederation of special interest groups. As such:
- Risk-taking is minimized and discouraged as the frequently repeated refrain of “no one gets fired for hiring (insert favorite large legacy company name)”. We must change this mantra and recognize the value of startups.
- Decision making is overly weighted on generating consensus rather than a defined set of strategic goals. This leads to the oft encountered experience in committees where a vote of 10 “yes’s” and 1 “no” is a “no”.
- Hyperfocus is on edge cases and exception handling. Healthcare administrators love to play “stump the chump” when evaluating new technologies. I think this comes mostly from our clinical colleagues who appreciate that exceptions and edge cases are important variables to consider when diagnosing and treating patients. However, in business process management, overly focusing on technologies’ failings in edge cases and exceptions can inhibit rapid adoption of helpful technology.
Industry has a Role to Better Foster Adoption: A Playbook for AI Innovators
Adam: In my experience, AI companies can do the following to facilitate adoption of their technology:
- Listen more, talk less: Empathy for the buyer is key in healthcare. Healthcare is the one of the most most difficult businesses – to operate, to sell into, and plan for strategically. There is tremendous “blurring of the lines” in the industry and new players (virtual first, retailers, physician enablement companies, Big Tech) creating enormous complexities for an industry known for its snail-like innovation capabilities. It deals with people at their worst in repetitive high stress situations within the most highly regulated environment. Lack of resources means prioritizing today’s emergencies over consideration of a new technology. Startups need to be sensitive to these daily challenges. By being an empathetic partner and not trying to “sell at all costs”, startups can become trusted partners and problem solvers. The goal is to move from vendor to trusted partner and the only way to do that is to have patience and be an active listener.
- Understand the business and customer: Too often entrepreneurs from healthcare think they can come into healthcare and solve its problems with ideas and solutions created outside of healthcare. The hubris or ignorance of some entrepreneurs to the complexity of the healthcare space has resulted in the untimely death of many startups. Spending time with customers to deeply understand their operating environment, challenges, and successes is the only way to find true product-market-fit and to develop a viable go to market strategy.
- Create a clear, concise value proposition with clear line of sight to significant cost reductions or revenue enhancement: In today’s financial environment, if a solution isn’t created to solve a regulatory need, then a hard ROI is essential. There is no free money floating around a health system today. If a startup wants to be considered a viable partner, they need to demonstrate real and ongoing savings in order to free up budget space for a long term contract.
- Provide transparency: Being a true partner requires humility and transparency. Startups need to be honest about their pricing, their product roadmap, and their current capabilities. Nothing damages a relationship more than overpromising and under delivering. People are forgiving of future features if you delivered on expectations from day one.
A Convergence of Factors
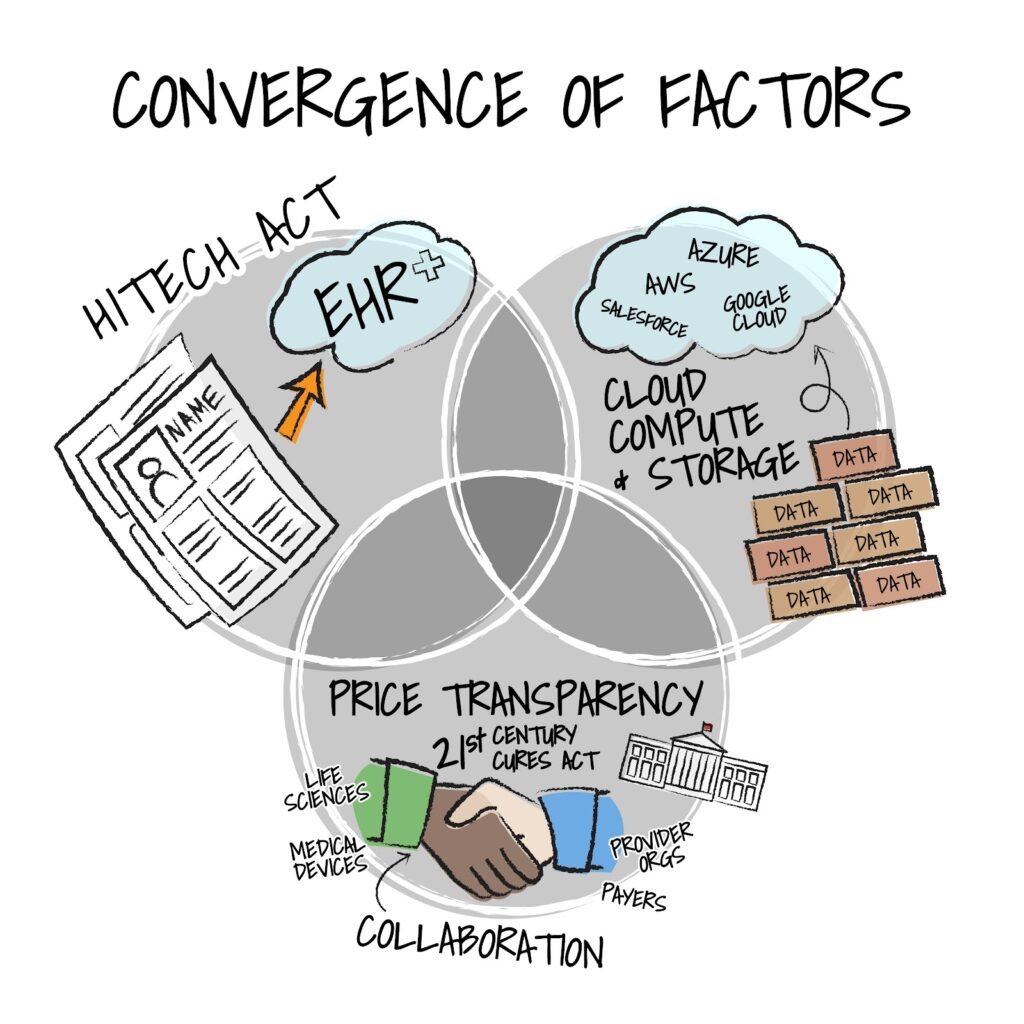
Eric: Despite the barriers outlined by my esteemed colleagues, the time does seem right for AI to have a moment. Why? Well, in a relatively short period of time (a bit more than a decade), three factors have converged driving innovation in the industry to new heights and possibilities.
First, the cost of big data has been crushed. The massive reduction in the cost of storage and compute have allowed health systems, physician practices, retailers, innovators, and incumbents to accelerate discovery and unlock insights from massive datasets.
The second factor, the implementation of the HITECH Act from ARRA (American Recovery and Reinvestment Act) resulting in the digitization of health records, has significantly increased the volume of health and wellness records in structured, digital formats. We’ve moved from single digit implementations of electronic health records to close to 100% of hospitals, practices, and ancillary services.
Finally, “favorable” government influence (we’ll save the details) of legislation is allowing access, facilitating value-based care, promoting interoperability, and fostering transparency. . As the largest “purchaser” of care the federal government certainly has the incentives to ensure we’re empowering healthier citizens while addressing costs – leveraging data, advanced analytics, and yes – many types of artificial intelligence.
SPONSORED BY AUGMEDIX
Healthcare is demanding enough. Clinical visit documentation only adds to the stress.
That’s why Augmedix Go helps busy clinicians by fully automating draft medical notes, allowing users to review the notes and upload them into EHRs in seconds.
It’s cost-effective, easy-to-use, and scalable to support busy clinicians across acute and ambulatory care settings.
Scale with your health system and start improving clinician efficiency today.
Real Examples of Implemented AI in Healthcare
Eric: Given Adam’s comments on the responsibility of vendor/partners, I thought it would be a good idea to highlight a few companies that seem to have cracked the code and have successfully implemented various types of AI at leading provider organizations.
- Decode Health (ML/Predictive) – the Decode Health data platform rapidly builds machine learning models with combinations of genomic, clinical, claims, social determinants, and other healthcare datasets. This accelerates precision medicine and research and development in support of biomarker discovery and the creation of new clinical decision support approaches necessary to predict and enhance patient outcomes.
- LUMINARE (ML/Predictive) – LUMINARE was founded to stop patients from dying of sepsis at home or in hospitals. They do this by leveraging the value of ML/Predictive Analytics in collaboration with human intelligence at the bedside.
- Augmedix (NLP/Generative AI) – utilizing natural language processing and generative AI models, Augmedix has developed a leading ambient clinical data capture capability which significantly reduces clinician burden associated with EHR documentation.
- Hippocratic AI (Generative AI) – General Catalyst and a16z backed startup building a safety focused LLM for healthcare with voice based applications to engage with consumers and complete a wide range of healthcare tasks.
- Digital Diagnostics (Computer Vision, ML/Predictive) – leveraging computer vision AI, the LumineticsCore product from Digital Diagnostics identifies patterns whereby ML models actually detect disease, significantly increasing access and reducing the cost to diagnose diabetic retinopathy & macular edema.
- Iterative Health (Computer Vision, ML/Predictive) – Iterative Health is pioneering the use of artificial intelligence-based precision medicine in gastroenterology, with the aim of helping to optimize clinical trials investigating treatment of inflammatory bowel disease (IBD) and improving the accuracy of colorectal cancer screenings. The company has developed ML models trained on images captured during colonoscopy procedures.
- Care.ai (Computer Vision, ML/Predictive/Generative AI) – Care.ai is enabling “smart” facilities (acute care hospitals, ambulatory clinics, skilled nursing facilities) leveraging computer vision, ML/predictive analytics, and generative AI to utilize data captured through ambient sources creating efficient, safe, and “aware” environments.
- DARVIS (Computer Vision, ML/Predictive) – is a virtual mapping application that combines computer vision and data management to resolve inefficiencies in supply chain for healthcare operations
- Epistemix (ML/Predictive – Generative AI) – using a synthetic population representing every person in the US, Epistemix enables payers, providers, pharmacies, and pharma to increase return on investmentI by simulating the impact of interventions, policies, and products being adopted by consumers across healthcare.
- Ronin (ML/Predictive) – with inputs from pharmacy data, clinical data, and social determinants of health data, Ronin is leveraging ML/predictive analytics AI models to identify oncology patients requiring intervention to manage treatment difficulties and lower costs as a result of clinical interventions
- Azra.ai (ML/Predictive) – accelerating the treatment of cancer by combining multiple sources of data, including computer vision image analysis, to ensure patient journeys are accelerated through various care episodes.
- Lirio (ML/Predictive – Generative AI) – combining behavioral science evidence with clinical and population health data, the company has trained reinforcement learning models to hyper-personalize communications (“precision nudging”) to ensure individuals make the best healthcare decisions and engage with health systems, providers, health plans, and others in the ecosystem to improve outcomes.
- Syllable (ML/Predictive, NLP, Generative AI) – improving administrative efficiency by automating the interface between patient and provider using conversational AI and training models to identify patients struggling to navigate the health system and elevate these findings to humans to correct.
These are just a few examples of companies that have demonstrated one or more successful chapters of the aforementioned “Playbook for Innovators” from my colleague Dr. Silverman – listening more, understanding the customer, a clear value proposition, and being absolutely transparent in the process.
A Few Final Thoughts on Healthcare and Artificial Intelligence
Eric: Healthcare has significant headwinds: an aging population, an aging workforce, serious competition for workers at the low end of the wage scale, and a surge in chronic disease straining the industry. AI has the potential to fill gaps and enhance efficiency – directly impacting operating margins and bending the cost curve for consumers and purchasers of care. From streamlining administrative tasks to assisting in diagnosis, AI can optimize workflows, allowing healthcare providers to focus on more complex and personalized patient care.
Lauren: Eric, I am worried about the involvement of AI in diagnosis unless we have a more thoughtful approach to better understanding the training and tuning of some of the AI models. I fortunately have seen this in action. I recently had the opportunity to catch up with Nick Archer, VP of Partnerships at Hippocratic AI (backed by General Catalyst and a16z) on a recent Friends of Project Healthcare podcast. Hippocratic AI is using reinforcement learning with human feedback using healthcare professionals (RLHFHP). This technology relies on clinical team members from Hippocratic AI and their health system partners to “grade” the responses generated from prompts of the proprietary LLM that Hippocratic AI is building. As Nick said “..we don’t want to ship a product that a clinician says is not ready for primetime. So we are actually hiring nurses and clinical professionals and we’re doing the RLHF (reinforcement learning from human factor) on these tasks that we’ve been discussing with clinical professionals…”
As I think about this, Hippocratic AI has a two sided model: their own proprietary LLM from trusted sources and a process of using RLHF with healthcare professionals. Together, this technology will move skeptical healthcare professionals to involved participants in the design and deployment of LLMs.
Adam: I will just finish with this thought: LLMs are needed now more than ever. In 1950, it was estimated that it would take 50 years for medical knowledge to double. By 1980, medical knowledge doubled every seven years and in 2010, every 3.5 years.
We now live in a world where medical knowledge doubles every 73 days.
Providers can’t keep up. We must embrace, and I believe we will, AI as a tool to utilize this growing medical information in a way that makes a difference for patients.
Eric, Adam, and Lauren: In conclusion, ****the prevailing narrative often leans toward skepticism, emphasizing the industry’s propensity to lag behind other sectors in adopting cutting-edge technology. However, a closer examination of the landscape reveals a compelling argument for healthcare not merely catching up but potentially leading the charge. The convergence of workforce challenges, the pursuit of equitable healthcare access, the implementation of next generation reimbursement models, and the disruption caused by digital health and retailers position healthcare to lead rather than lag in AI implementation and integration.
We’d love your comments and feedback, and you can count on the three of us to continue the conversation…
If you enjoyed this, consider subscribing to Hospitalogy, my newsletter breaking down the finance, strategy, innovation, and M&A of healthcare. Join 20,000+ healthcare executives and professionals from leading organizations who read Hospitalogy! (Subscribe Here)