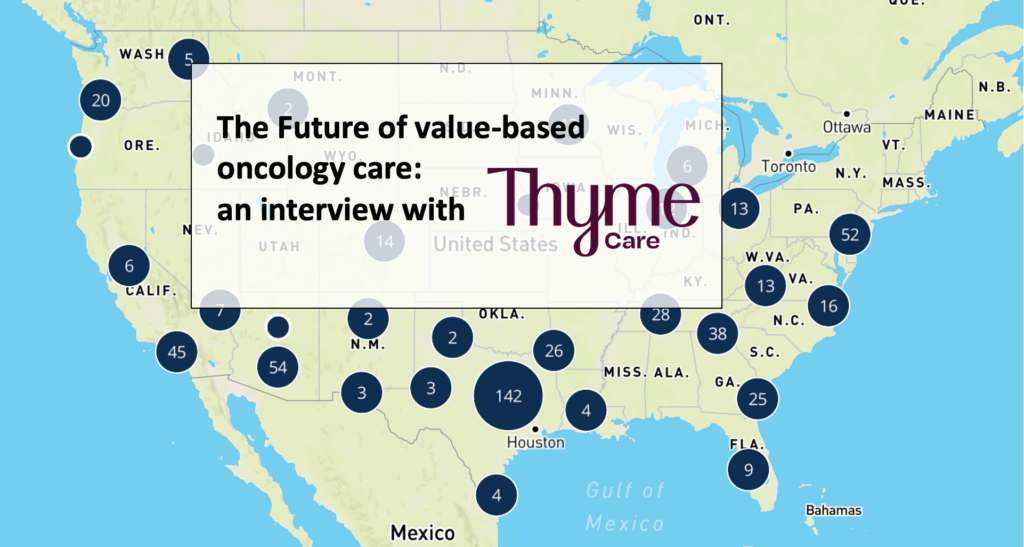
I’m very interested lately in value-based specialty care in arenas where it makes sense, and one of the more interesting spots I’m watching is in oncology with CMMI’s Enhanced Oncology Model (’EOM’) that kicked off over the summer.
I was lucky enough to interview some members of the Thyme Care team earlier this year in what was meant to be a deeper dive on the space (and ultimately didn’t come to fruition).
Still, I wanted to share Thyme Care’s Dr. Bobby Green and Scott Voigt’s thoughts on the future of value-based oncology care – since they were gracious enough to spend some time answering my questions and provided some really interesting background on the past, present, and future for Oncology care, an area of high spend within healthcare.
Keep Thyme Care on your radar. Since this conversation, Thyme Care went on to partner with the American Oncology Network to foster its clinics’ participation in the EOM. Thyme then raised $60M in a late August Series B fundraise co-led by Town Hall Ventures and Foresite Capital.
Let’s dive in!
SPONSORED BY BLAKEMORE CONSULTING

Building an adequate provider network is crucial for ensuring members’ access to care.
But it’s far from easy.
That’s why payors of all sizes turn to leading turnkey network development firm Blakemore Consulting for all things network adequacy, development and management.
Blakemore Consulting brings a specialized approach to all services including:
- Provider network builds
- Network analysis and strategy
- Provider contracting and recruiting
- Adequacy reporting and modeling
With focused project planning capabilities, targeted provider prospecting skills, and experience with state-specific adequacy requirements, Blakemore helps you navigate building provider networks with ease.
The Enhanced Oncology Model had a predecessor, the Oncology Care Model – what went well, and what went wrong from the OCM?
The Oncology Care Model (OCM) really changed the conversation around value based care in oncology. Despite some of its limitations, the OCM in many ways changed how the oncology community talked about value based care. There was widespread participation across many practice types, and for many oncologists it was their first real experience practicing in a value based framework. It relied primarily on administrative claims data to define episodes of care and gauge cost savings against predominantly historical benchmarks. Claims data does not provide specific information related to one’s cancer diagnosis, histology, molecular characteristics, disease stage and similar. This dynamic led to poor specificity of a cost benchmark against real cancer treatment episodes. Oncology practices, especially smaller ones, with an adverse case mix could be unfairly penalized.
While the OCM included a trend factor to account for the introduction and use of novel therapies (which are universally very expensive), this factor was applied at the practice level rather than at the disease level – again causing problems with case mix.
Both OCM and comparison practices saw total episode costs rise over the course of the model. This suggests that the proportion of an episode that is truly impact-able is shrinking over time. Performance-based risk for drugs suggests that clinicians have discretionary power over prescribing, which does not jive with the fact that oncology is a field as heavily dictated by clinical guidelines and compendium-listed regimens as it is.
What’s changing with the Enhancing Oncology Model and what does it unlock that is different from OCM?
EOM is a more focused version of OCM, but it has some significant differences. This includes:
Join the thousands of healthcare professionals who read Hospitalogy
Subscribe to get expert analysis on healthcare M&A, strategy, finance, and markets.
No spam. Unsubscribe any time.
- A smaller, higher risk patient population
- Mandatory risk
- Added requirements (ePROs and Health Related Social Needs (HRSN) screening) which make the program more operationally complex for practices to execute
- Disease specific factors within the performance methodology
- Lower Monthly Enhanced Oncology Services (MEOS) payment
CMS has designed the thresholds for performance based payment to be higher for practices to meet (practices need to achieve a 2% minimum reduction in total cost of care before they can unlock shared savings) in the EOM. Further, a larger proportion of shared savings flows back to CMS than in OCM.
EOM collects more data about social determinants of health, electronic patient-reported outcomes, etc – more patient voice in treatment plan and care. But reporting requirements are considerable.
Value-based specialty care is becoming more and more of a thing. What is it about Oncology that makes it more palatable to value-based care arrangements?
Oncology is the highest per-capita spend in all of medicine. It is extremely prevalent, oftentimes treated not as an episodic thing, but as a chronic disease. This is particularly true for metastatic disease, but even increasingly for earlier-stage diseases given the rise of ‘maintenance regimens’.
Because there is lots of variability in spend and quality across demographics and regions, there are opportunities to improve both the patient experience and the total cost of care through targeted interventions around early palliative care, proactive symptom management, and care navigation.
As a follow-up, what’s the current state of oncology and what makes value-based care difficult? Are reimbursement models like the EOM even the right avenue to pursue?
The vast majority of oncology care today is delivered in fee for service models. While there is a large amount of cancer spend that might not be addressable, especially some of the drug spend, there is still both drug and non drug spend, where there are opportunities to deliver higher value care and lower the cost of care. Care navigation, for example, is important to value-based care but it is not widely reimbursed.
EOM is really important to drive VBC and improve outcomes because:
- Like we saw with OCM, CMS launching a program changes the conversations around FFS vs VBC in positive ways. It gets people motivated to try new things and succeed in value-based oncology care.
- It gives more oncology practices experience in VBC, which is really important to improve outcomes and reduce costs.
There are good and bad things about the EOM model, but it provides the industry with an opportunity to learn what works. Despite possible flaws, it’s the right avenue to pursue and we believe the pros (better health outcomes and reduced costs) will outweigh the cons (logistical burden) in the long run.
Where are the highest cost areas of oncology and how does the EOM address these areas (e.g., drug spend)?
- By including drugs in the total episode costs, EOM explicitly makes these costs the responsibility of participating practices and physicians.
- Drugs are the highest cost areas but there is still significant spend around acute care utilization, end of life spend, and other areas
- Biosimilars, generics, other things that can be done that can impact drug spend:
- Therapy at end-of-life (EOL) when its not aligned with patient goals
- EOL care, acute care utilization
See more in our blog post on financial toxicity in cancer here.
Who’s participating in the EOM and what are the incentives to participate? What tools do practices need to participate?
A little over half of EOM participants having previously participated in the Oncology Care Model (OCM). This signals that practices have mixed feelings about value-based oncology care and/or the EOM model.
Some are doing it because they feel confident that they can come out on top with shared savings (few go into medicine to try and arbitrage actuarial risk in their practice), but others are increasingly recognizing that getting experience under their belt with value-based care is going to be key into winning new contracts, particularly as more and more commercial payers are also seeking to partner with practices that have this experience.
In our view, the upsides of EOM include:
- It gives oncologists an opportunity to participate in VBC, which we think is important
- It is voluntary to participate in; those that do will be seen as more innovative, and have the ability to try out VBC models before it becomes mandatory
- It gives practices an opportunity to learn what works and what doesn’t; and adjust from there
The downsides of EOM are:
- It is operational complex and there are dollars on the line
In order for practices to participate, they need to be able to provide care navigation and track social-related health needs and electronic patient reported outcomes. That level of insight, combined with understanding the cost drivers being able to operationally track the patients going through the practice, requires a fair amount of analytic expertise. In our view, practices will be challenged to succeed in EOM unless they bring on a dedicated value-based enabler that can alleviate the operational complexity from practices and provide the analytic support, so they can instead focus on providing the highest quality patient care.
SPONSORED BY ADONIS
Time and time again, we’ve heard about how challenging it is to keep up with the velocity of changes that impact physicians. Policy, legislation, adjudication rules, Medicare/Medicaid standards, revenue cycle, and more are prime examples.
Luckily, Dr. Jared Dashevsky, Resident Physician at Mount Sinai and Co-founder of Healthcare Huddle is here to help.
Adonis is teaming up with Jared to host an exclusive 1:1 conversation on November 14th at 2PM EST to explore the challenges that physicians are facing, ranging from legislation, revenue cycle management, navigating prior authorization, and finding harmony with private equity partners. Putting private practices and physicians on the operational front foot is our shared mission.
Trust me, you don’t want to miss it. Register Today.
What should investors and operators know about the Enhancing Oncology Model before jumping in?
When it comes to value-based models, cancer care today is where chronic kidney care was five or more years ago. And, just as success with chronic kidney patients relies on a kidney-focused care model that is integrated with the nephrologist, cancer care can be greatly enhanced by deploying oncology-focused clinical navigation in partnership with oncologists.
For investors, there is significant upside in investing in value-based care enablers (like Strive Health in kidney care, Thyme Care in cancer care). As the healthcare industry continues to shift from FFS to VBC, we will see more niches follow suit after primary care, kidney care and cancer.
For providers, it’s very difficult for them to address the multi-faceted needs of their patients while keeping pace with the number of patients they have to see, especially as the supply of specialists continues to be under pressure. They should consider value-based partners to help make that kind of support possible while reducing the need for avoidable and costly acute care services.
Value-based care transformation in cancer requires more than just aligned financial incentives, it requires a deep understanding of where the opportunities for enhancement and cost-savings lie, an emphasis on reduction of acute care utilization, and an appreciation for novel solutions such as patient navigation that payers and practices may find difficult to fund and build in-house.
Will the EOM move the needle ultimately? In what aspects?
Value-based cancer care hasn’t reached a “tipping point” yet, but we believe EOM will further the conversation with oncologists, and that it is a positive step forward. EOM changes the conversation about value-based oncology care, and we believe it will have a ripple effect that will lead to the next step. Next we will see commercial payers thinking about value-based care on a population health level, and experimenting with models of their own.
As we’ve seen with kidney care, CMS can be seen as a forcing function and is going to have influence. But in order to succeed in EOM, practices should consider bringing on a dedicated enabler to focus on care navigation and coordination, rather than try to build it from the ground up (and assume the operational complexity on their own).
What’s next on the horizon for oncology in general?
When we talk about what’s next for oncology, very often we hear about new therapies and medical innovations. This is the strength of American medicine. We’re proficient at inventing and leveraging advanced technologies and harnessing vast resources in pursuit of scientific breakthroughs, especially during crises or because of urgent need. But any medical victory over cancer will be greatly diminished if we do not also achieve commensurate improvements in access, experience, and quality of life for cancer patients and survivors. [See our recent op-ed in Fortune about this].
Improving the patient experience is one of the pillars of value based care, so it’s exciting to see more progress towards achieving this goal, and recognize that EOM is one part of it.
Thanks for Reading!
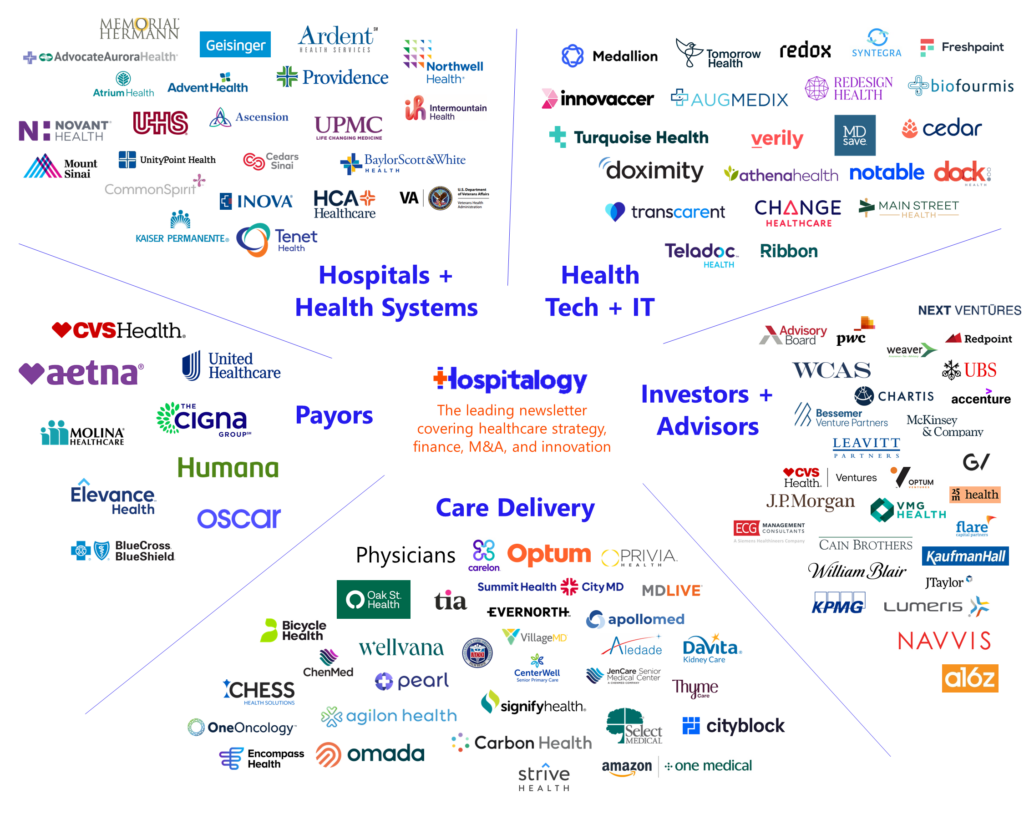
If you enjoyed this, consider subscribing to Hospitalogy, my newsletter breaking down the finance, strategy, innovation, and M&A of healthcare. Join 23,000+ healthcare executives and professionals from leading organizations who read Hospitalogy! (Subscribe Here)