The Hospitalogy guest posting series continues with a great piece from Notable Health’s CMO and longstanding healthcare exec Dr. Aaron Neinstein!
SPONSORED BY VERIFIABLE

SPONSORED BY VERIFIABLE
Rigid compliance is fundamental to providing safe, high-quality, and ethical care.
That’s why Verifiable’s NCQA-compliant credentialing technology automates 99% of primary source verifications – for enhanced reliability and accuracy of provider data.
By keeping organizations informed of requirements and industry best practices for strong audit-readiness, Verifiable empowers them to:
- Establish a credentialing committee
- Develop and implement effective credentialing policies and procedures
- Access all necessary data for NCQA compliance, including NPDB
Ready to take control of credentialing procedures, feel confident with compliance, and scale operations with ease?
Take Control of Your Credentialing
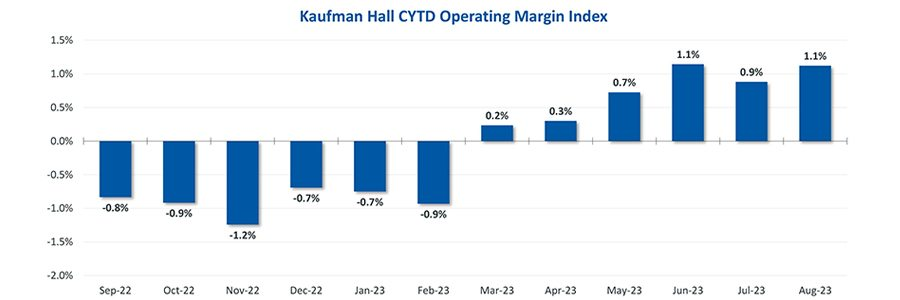
After several turbulent years, many aspects of healthcare delivery have begun to stabilize. Kaufman Hall’s latest Hospital Flash Report shows that US hospitals have an overall trend of positive margins in 2023, which is in stark contrast to the previous couple of years. Granted, margins today are still below historical averages, but health system executives do see an improved outlook.
Source: National Hospital Flash Report: September 2023, Kaufman Hall
These data align with much of the sentiment coming from health system leaders from across the country. Last week I had the opportunity to speak with and learn from more than 70 leaders from health systems of all shapes and sizes. Through these discussions, I was interested in finding the common threads, the challenges that cut across the industry, and the approaches that are finding success. The following are the top themes that health system leaders are thinking about now and as we head into 2024.
Moving from AI hype to AI help
Without question, the hottest topic of conversation in healthcare, and across most industries, is artificial intelligence (AI). Recent research from Bain & Company and KLAS Research highlights the point. The firms found that 70% of health system respondents believe that AI has reached a turning point in its ability to reshape healthcare. AI is a regular C-suite conversation, and if you are a healthcare executive, no doubt your hospital board is on your case asking you about AI. The rise of large language models (LLMs) and the consumer adoption of ChatGPT have moved the buzz to a fever pitch. According to Bain & Company, only 6% of health system executives say their organization has an established generative AI strategy. That’s going to change, rapidly, in the coming quarters.
Many are thinking about how AI can be put to use to change the nature of healthcare jobs, to support and augment care teams, moving beyond digitization. For example, rather than shifting a prior authorization from paper to electronic, health systems are thinking about using AI to eliminate staff effort on authorizations. And for good reason. Burnout continues to be a significant issue facing doctors, nurses, and clinical staff. Even pre-pandemic, conservative estimates found that approximately $4.6 billion in costs were related to physician turnover and reduced clinical hours that could be attributed to burnout each year in the United States. This month, JAMA Network reported on new research that found that physicians who experience less overall burnout tend to spend less time on administrative tasks. Nobody should need to hunt for a use case for AI. The promise of AI lies in its ability to solve real problems – unlocking opportunities to tackle challenges that have seemed intractable to date.
The 2000s saw those companies that took advantage of the web leap ahead. The 2010s saw those companies that took advantage of consumer experience and digital leap ahead. This decade will see those companies that take advantage of AI leap ahead.
Organizational and governance models for AI
When it comes to moving beyond the hype in deploying AI, much of the focus is rightly on how health systems should organize around AI and how best to think about governance for such a powerful and nascent set of technologies. Much of the digital transformation work happening today has AI at the center. According to McKinsey, while 90 percent of companies have launched some flavor of digital transformation, only a third of the expected revenue benefits, on average, have been realized. Why? McKinsey hits the nail on the head when it says that “digital transformations are, first and foremost, people transformations.” Transformation is about using technology to generate better analytics and insights into the customer experience, enabling more continuous iteration and improvement of products, services, and experience to meet customer needs.
Several of the executives I spoke to acknowledge that healthcare has traditionally been organized and operated in silos. Most haven’t integrated technology across core business processes and have not brought business, technology, and operations together in such a way to drive transformation. Bold health system leaders are pushing their organizations to think horizontally instead of vertically, recognizing that transforming a workflow requires looking across traditional functions, and looking at end-to-end customer or staff experiences and journeys, through the lens of the customer as opposed to an internal lens.
Join the thousands of healthcare professionals who read Hospitalogy
Subscribe to get expert analysis on healthcare M&A, strategy, finance, and markets.
No spam. Unsubscribe any time.
Recently, I spoke with Ilana Golbin, Director and Responsible AI Lead, at PwC, who said, “I don’t believe, at all, that a good governance program is a hindrance to innovation. I think it’s an accelerant for innovation.” She analogized this to traffic rules of the road, believing that establishing clear guardrails and safety frameworks allows teams to move forward with clarity and certainty, rather than constantly stopping and looking around to make sure they are proceeding safely.
AI governance has to be closely coupled to the organizational strategy according to Golbin, and it should be driven by the ethics and values that the organization is looking to uphold. Rather than running to develop a new AI governance approach, Golbin advised that institutions already have mechanisms in place for things like compliance, risk management, safety, privacy, and security that should be leveraged, adding some unique components for AI rather than starting from scratch.
SPONSORED BY FUNDRISE
We all know AI will change the future of healthcare.
That’s why I’m partnering with Fundrise to help you capture some of the upside.
Fundrise empowers investors of all sizes to invest in top private, pre-IPO AI companies, all in five minutes or less.
Want in? Join 2 million investors and start investing in Fundrise today. #fundrisepartner
Technology as a competitive differentiator
In the previously mentioned survey of 201 US healthcare provider executives conducted by Bain & Company and KLAS Research, 56% cited software and technology as one of their top three strategic priorities. What’s more, 75% of respondents said they expect growth in software and technology spending to continue over the next 12 months. These data points make it clear that health system executives view software and technology as competitive differentiators.
This comes at a time when the number of competitive threats to health systems is expanding. Both traditional and non-traditional care providers, including retail and technology giants like Amazon and Walmart, are working to provide patients with more choice in where and how they get their care. Two tactics are gaining traction among health system executives as they seek to evolve and enable patient acquisition, loyalty, and retention in the current climate.
The first is using AI to drive a level of personalization that, while common in retail, travel, and even financial services, has not previously been possible in healthcare. With upwards of 80% of healthcare data being unstructured, the ability to understand, analyze and action this data at scale was not historically possible. In this case, rather than personal recommendations on what to buy like Amazon, we can personalize patient experience at scale by allowing clinicians to proactively guide each patient on their unique care journey.
Identifying and closing gaps in care is one area where this is already happening in a tangible way. By automating the process of scrubbing patient charts and putting LLMs to work, health systems can identify care gaps and send personalized outreach to patients to schedule care to close those gaps. With AI doing the heavy lifting, much of this work can be done without requiring additional staff and even without staff intervention.
The second tactic is using technology to tackle rising labor costs fueling recent financial challenges. Recent years have continued to see an administrative creep in healthcare, with the deployment of technology thus far unable to bend the curve of rising labor costs. Health system leaders acknowledge that they cannot continue to solve problems by adding more people. Jeri Koester, CIO of Marshfield Clinic Health System, describes a conversation a few years ago where they realized “we can’t hire our way out of this,” and their philosophy was “How can technology engage another group of people who can help improve care… they’re called patients.” In addition to more self-service capabilities for patients, health systems are looking at process automation to enable their staff to work more productively, to top of license.
Courageous leadership
Healthcare organizations are in a hard place. Financial challenges remain, workload burdens exist, staff burnout continues, consumer expectations are rising, and uneven quality outcomes are very real. To take on transformation, we heard from leaders across the country that it requires courage, boldness, and risk-taking. In an industry where it is very easy to keep doing the same thing, and for things to be the way they have always been, it is much harder to stick your neck out and do something new and different.
We heard about several tactics in driving transformational change, including the power of storytelling, as well as the phrase “just try it.” The latter refers to reminding staff fearful of change that it isn’t harmful to just try something small and that it can always be undone. From there, you try a little more and a little more and a little more.
One leader noted that imagination is good for healthcare and I was particularly struck by the notion, shared by yet another health system executive, that if you’re not making people uncomfortable, you’re not transforming anything.
Courageous leaders will find ways to try, to learn, to iterate, and will build this mentality and risk tolerance into their cultures. They will remind their organizations that the current state of healthcare is not a great alternative, and as Joe Biden said, “Don’t compare me to the Almighty, just compare me to the alternative.”
About the Author
Dr. Aaron Neinstein is the Chief Medical Officer at Notable, the leading intelligent automation company for healthcare. In this role, he employs his care delivery expertise to strengthen Notable’s product strategy and roadmap, ensure high-value customer outcomes, and foster healthcare community engagement on the value of AI and automation for patients and care teams.
Before joining Notable, Dr. Neinstein spent over a decade as a physician executive in digital health and informatics, most recently as Vice President of Digital Health at UCSF. At UCSF, he previously played an integral role in leading their Epic EHR implementation. He is a Fellow of the American Medical Informatics Association and a federal appointee to the US Health Information Technology Advisory Committee (HITAC). Dr. Neinstein has received accolades such as the UCSF Excellence in Teaching Award and is a frequent speaker and media contributor. He has authored numerous peer-reviewed articles in journals like JAMIA, Nature Medicine, and NEJM Catalyst.
Triple board-certified in Endocrinology, Clinical Informatics, and Internal Medicine, he is a national authority on diabetes technology. He co-founded Tidepool, a non-profit building tools for diabetes management. He continues a part-time clinical practice in Endocrinology at UCSF, focusing on diabetes care, and holds a faculty appointment as Associate Professor.