There’s been discussion around physician-owned hospitals (POHs) after Senator James Lankford reintroduced a bill – the Patient Access to Higher Quality Health Care Act (PAHQHCA – unreal) – that would repeal the ban on POHs.
More recently, this rhetoric has been heating up, eliciting a response from the AHA:
- This study indicating physician owned hospitals could save Medicare over $1B;
- Why the AHA is vehemently opposed to physician owned hospitals and its stances; and
- Continued conversation in Congress mulling over the idea of lifting the moratorium on POHs to improve access
So I figured, why not dive into the two sides of the debate today?
As a reminder, this post is a thought experiment. With any hot topic in healthcare, there is plenty of nuance to consider that one newsletter simply can’t get to.
Join 18,000+ executives and investors from leading healthcare organizations including Privia, ApolloMed, and HCA Healthcare, health systems including Providence, Ascension, and Atrium, as well as leading digital health firms like Cityblock, Oak Street Health, and Turquoise Health by subscribing here!
SPONSORED BY VERIFIABLE

Ask anyone familiar with outdated credentialing practices…
It’s not fun. Paperwork, manual data entry, high-margin for error. The list goes on.
Introducing Verifiable.
With Verifiable, credentialing happens 4x faster than with manual processes. 99% of license verifications and ongoing monitoring are automated and primary source verifications are completed in seconds.
As a flexible healthcare API, Verifiable also enables effortless customization to meet your specific needs, and seamless integration into your existing systems and workflows.
Make the switch, witness the transformation, and leave outdated credentialing methods in the past. Ready to experience the difference?
[Book a Demo]
Key Takeaways on the Physician Owned Hospital Debate
The ACA placed a ban on Medicare-certified physician owned hospitals in 2010. Physicians and proponents want that ban repealed. Hospitals and opponents want it to stay. The ACA facilitated consolidation in healthcare which has exacerbated the conflict between corporate interests and physicians.
Proponents of the ban argue that physicians would cherry-pick commercial patients and distort financial incentives for physicians, who control patient referrals.
Critics of the ban argue that POHs would level the playing field between corporate players and physicians as well as reduce hospital consolidation by introducing competition to concentrated markets. They also argue that hospital market power has resulted in bargaining power over physicians in the past decade-plus.
Healthcare should be physician-led, and the POH trend ultimately speaks to the notion that physicians perhaps don’t feel heard in board rooms or policy decisions happening in healthcare across the country.
Context for the Physician Owned Hospital Debate
Prior to 2010, physicians could own equity in hospitals. That included general acute care hospitals as well as specialized surgical hospitals. For a full picture of the history of POHs, Health Affairs did it better than I ever could here. TL;DR – there was a lot of concern with POHs and physician self-referral which led to Stark Law regulation and the eventual ownership ban.
Join the thousands of healthcare professionals who read Hospitalogy
Subscribe to get expert analysis on healthcare M&A, strategy, finance, and markets.
No spam. Unsubscribe any time.
Along with that historical context, there are a number of other factors happening in healthcare right now that have reinvigorated POH efforts:
- Hospital markets are concentrated – 67% of metro markets are considered ‘highly concentrated’ according to the Health Care Cost Institute. Sponsors of the bill think that introducing POHs would help with that concentration
- The corporatization of physicians is at an all-time high – 80% of physicians are employed by a hospital or corporate entity. Physicians and proponents feel that they deserve a fair playing field for hospital ownership. And they’re utterly sick of corporate interests in healthcare. Trust me, I’m on Twitter – I know.
- At the same time, physician compensation is facing increased uncertainty amid reimbursement pressures. Compensation is not keeping up with inflation, a point that physicians bemoan.
Post-POH, a more common form of ownership among physicians these days is in ambulatory surgery centers (ASCs) given that there is a Stark exception for the outpatient surgery option. There are a fair number of rules associated with physician ownership in ASCs along with financial distributions (e.g., equity owner has to perform a third of his or her procedures at the ASC; buy in and buy out can’t be based on volume; distributions are based on equity and not on volume; etc.).
The House introduced a bill in 2017 for a similar purpose to repeal POH moratorium on ownership.
Viewpoint 1: Physicians should own hospitals
As a result of these prevailing dynamics in healthcare, Senator James Lankford reintroduced the act this week. In a WSJ opinion piece, he and Brian Hill highlighted hos POHs would increase competition and enhance the entrepreneurial spirit of physicians. I’ve inserted pointed quotes around how the dynamic in healthcare and how Bankman and the co-sponsors believe the current dynamic doesn’t make sense:
“What if lawyers weren’t allowed to own law firms or chefs weren’t allowed to own restaurants? Sounds absurd, but it’s a reality for one profession: doctors.” – WSJ Opinion
Another opinion piece from the Hill echoed similar sentiment:
“So, while a baker can open a bread factory and a lawyer can found a legal firm, a physician can’t open a hospital.” – The Hill Opinion
Ultimately, the view in favor of POH is that it evens the playing field. From the AMA:
“Physician-owned hospitals have been shown to provide the highest quality of care to the patients they serve, he noted.
They are consistently among the top hospitals recognized for high quality care and patient satisfaction under the Hospital Value-Based Purchasing (VBP) Program, which the Centers for Medicare and Medicaid Services (CMS) administers. Despite physician-owned hospitals accounting for just 5 percent of hospitals that participate in the VBP, seven of the top 10 performing hospitals and 40 of the top 100 performing hospitals were physician-owned in the 2017 fiscal-year rankings.
And when Physician Hospitals of America, an association for physician-owned hospitals, analyzed CMS payment data, it found that these facilities saved Medicare $3.2 billion over a decade.”
Viewpoint 2: Physicians should NOT own hospitals
The AHA holds the consensus view on why physicians shouldn’t own hospitals, outlined in the factsheet published here. Main talking points include:
- POHs don’t provide emergency services and other low-margin care services
- Physicians self refer and that leads to higher costs for the healthcare system; it’s a conflict of interest that results in unnecessary, more expensive care for patients and payors
- POHs cherry-pick commercial and the most profitable patients: “MedPAC and GAO found that physician-owned hospitals treat fewer Medicaid patients. This trend creates a destabilizing environment that leaves sicker and less-affluent patients to community hospitals, threatening the health care safety net.”
- Shutting down POH ownership resulted in $500M in savings according to the CBO, in direct conflict to the report shared by the AMA in the opposing viewpoint above. Healthcare is fun, isn’t it?
“Research findings thus far confirm that physicians’ ownership and referral present conflicts of interest through medical and economic patient selection and potentially excessive utilization. The policy response must prevent these results and preserve fair competition among hospitals.” – Health Affairs, 2006
Blake’s Take
Similar to my thoughts on Certificate of Need laws, I side with the “let’s make markets more competitive and free” side of the equation. Ultimately, physicians should have the right to own and operate hospitals, and the arguments put forth by the opposing side (for the most part) don’t seem to stand well today. For instance, if certain strategies including building MOBs in heavy commercial areas and tracking the capture rate of employed physician referrals into health systems, aren’t those arguments against POHs moot? If traditional healthcare systems are doing these things anyway, then it doesn’t make sense to prevent a group of physicians from doing so, too. It’s regulatory capture rather than competition.
That being said, the POH debate is delicate. Consider the comparison of a physician to a baker. Terrible metaphor. Your local baker isn’t a highly trained expert consulting with you in extremely complex nuanced cases. Your baker also knows the price of his loaf of bread and doesn’t have authoritative command or direction over what loaf you buy. If he tells you that you need 10 loaves of bread, that doesn’t mean you’re gonna buy 10 loaves of bread. You probably know that you don’t need that many loaves.
The physician-patient relationship is quite different from most other industries considering inelastic demand of healthcare services and information asymmetry. That’s why physicians and nurses are some of the most trusted professions on the planet. You trust your family doctor. Or the surgeon about to cut you open. For these reasons, we have to be thoughtful about the financial incentives we present to physicians. Healthcare should be physician and clinician led, but let’s make sure we get it right this time with policy.
Just like any other part of healthcare, there are good actors and bad actors. Because physicians control so much of healthcare (patient referrals, demand generation through services and diagnostics), if we open up Pandora’s Box of POHs, there are ramifications to consider. We have to remember that there are plenty of physicians that like money too (and deserve to be compensated, don’t get me wrong). If physicians owned hospitals, they would hold heavy financial incentive to refer everything to the equity-owned, higher cost, higher dollar hospital setting.
How would POHs affect investment and total cost of care in 2023? Would the shift to outpatient settings get squashed as physicians transition from ASCs to hospital-based care? Would the risk movement stop in its tracks? The battle between payors and providers would get even worse.
And then let’s consider private investment. The floodgates would open. Private equity players would quickly and immediately raise funds to invest and roll-up physician owned hospitals, promising higher returns for physicians and managing the admin and back office functions. Physicians not wanting to run day to day operations would hand off responsibilities to corporate interests and management companies, chase higher rates and higher dollar procedures in an extremely effective fashion.
The physician owned hospital rallying cry is an interesting trend thought experiment to consider, and as with anything in healthcare, there is a ton of nuance to consider here. There is plenty I’ve missed. If you have any thoughts around the physician owned hospital debate, I’d love to hear your commentary. Shoot me an e-mail at [email protected].
Resources:
- Reversing Hospital Consolidation: The Promise Of Physician-Owned Hospitals (Health Affairs)
- End ObamaCare’s Ban on Physician-Owned Hospitals (WSJ)
- Ambulatory surgery center ownership models (NCBI)
- Fact Sheet: Physician Self-referral to Physician-owned Hospitals (AHA)
- Why can’t doctors own hospitals? (The Hill)
- Is it time to lift the ban on physician-owned hospitals? (MedEcon)
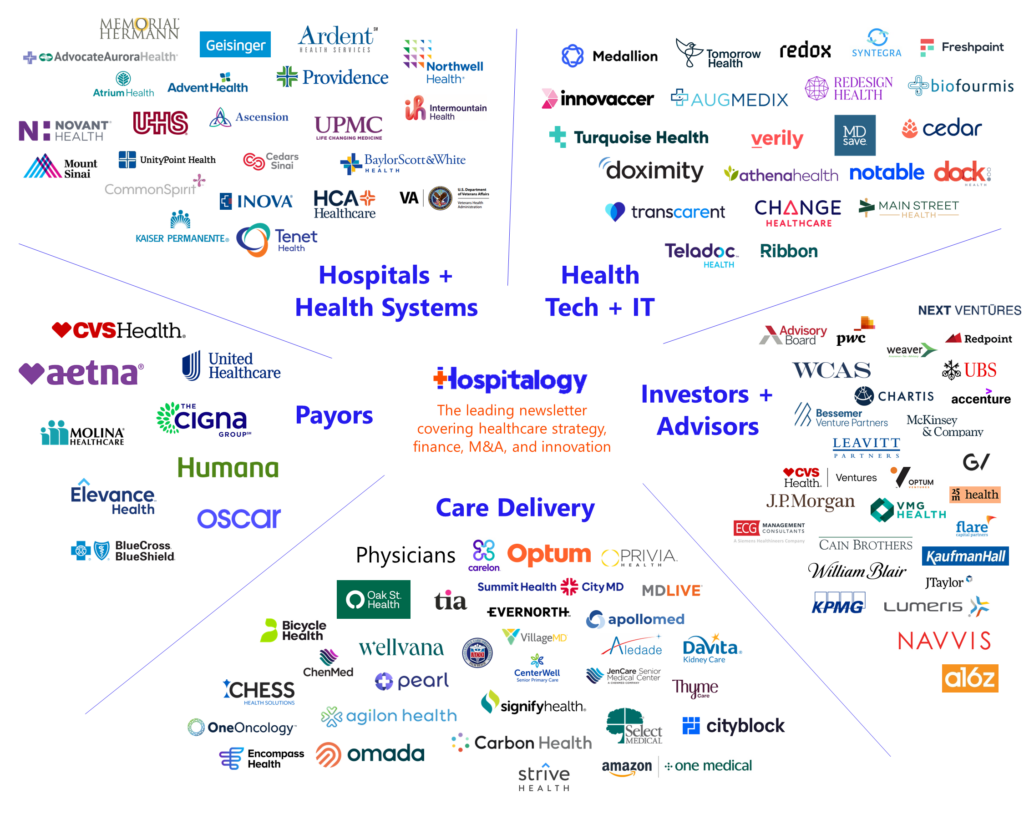
Join 18,000+ executives and investors from leading healthcare organizations including Privia, ApolloMed, and HCA Healthcare, health systems including Providence, Ascension, and Atrium, as well as leading digital health firms like Cityblock, Oak Street Health, and Turquoise Health by subscribing here!

