HUDDLE INSIGHTS
Mental Health Care in 2032
Mental health care in 2022 is good but not great. If we compare the progress of mental health care to the progress of the automobile, we just figured out the assembly line to get more cars to more people.
Given that I recently finished my psychiatry clerkship and May is Mental Health Awareness Month, I thought it’d be fitting to share what I envision mental health care will look like in 2032.
Background
Statistically speaking, around 2,500 of the 12,000 people reading this newsletter have a mental illness. This mental illness can range from mood disorder to anxiety disorder, substance use disorder to personality disorder. This is all to say:
- Mental illness is common.
The pandemic has only exacerbated mental health problems, with the most recent study showing a 25% increase in the prevalence of depression and anxiety worldwide. Burnout is another problem. The pandemic has pushed frontline health providers to emotional exhaustion, depersonalization and compassion fatigue.
So, mental illness is common. But solutions to addressing mental illness are lacking, given the shortage of mental health technology, poor access to mental health providers and the general unknowns of mental health.
The Year is 2032
The year is 2032. I’m finally a physician practicing on my own. What does mental health care look like?
Wearable Technology
Right now, there are as many people who own a smartwatch as there are people with a mental illness. Wearable tech is currently focused on using data like heart rate or heart rate variability to predict body stress levels. For example, I exercise intensely for an hour and my wearable (WHOOP) recognizes this as high bodily stress. But what about mental stress?
I envision wearable technology will be able to analyze data to predict mental stress. I use the word “mental stress” to encompass symptoms of mental illness such as excessive fatigue, anxiety, depressed mood, or decreased interest in activities. WHOOP is already inching towards the “mental stress” component—every couple of weeks, they send me a survey as soon as I wake up asking me questions about my mental health, which come from the PHQ-9 depression survey.
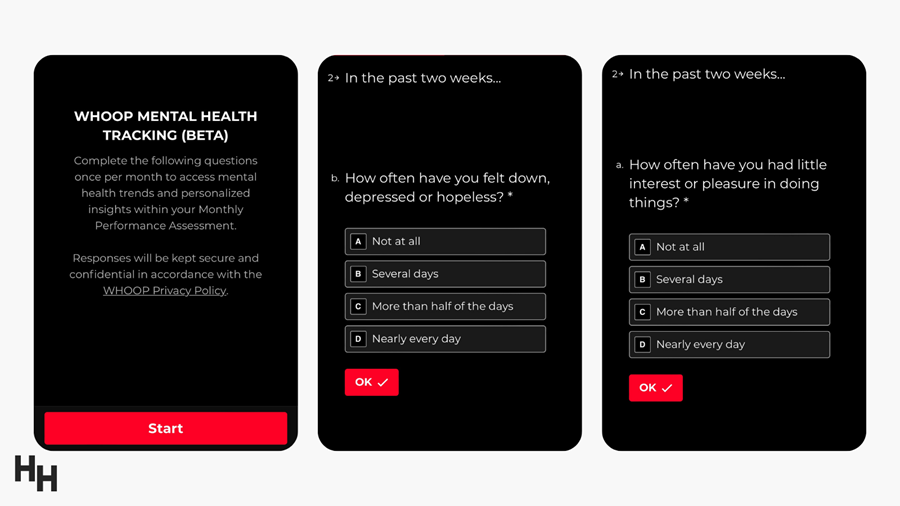
I imagine that if my score starts trending upwards, WHOOP will alert me saying:
Hey Jared! We’re seeing a trend that you may be feeling more down than usual. Consider reaching out to a mental health provider.
To take it a step further, WHOOP can detect specific prodrome symptoms of mental illness such as mania. For example, say I have bipolar disorder and WHOOP sees that, over the past week, my sleep has been decreasing and my activity level (measured by average daily HR) has been elevated. WHOOP could alert my psychiatrist that I may be having a manic episode, allowing my psychiatrist to intervene STAT.
Overall, I envision wearable tech playing a pivotal role in mental health. Wearables will be able to detect depression, burnout, mania, anxiety (panic attacks)—you name it.
A New Approach to Therapy
“Who’s your PMCP?”
“My what?”
“Your primary mental care provider?”
Join the thousands of healthcare professionals who read Hospitalogy
Subscribe to get expert analysis on healthcare M&A, strategy, finance, and markets.
No spam. Unsubscribe any time.
In 2032, people will view mental health with as much importance as their cardiovascular health. Just like (I hope) everyone has a PCP, everyone will have a PMCP.
Everyone has access to telehealth technology, meaning everyone has access to providers. I envision the PMCP is a licensed therapist who provides psychodynamic therapy and does so virtually. You use their services as much or as little as needed, but just like you have an annual check-up with your PCP, you’ll also have a yearly check-up with your PMCP. Patients will be screened for trauma, depression, anxiety, and burnout during this check-up. If the PMCP finds something alarming, they can refer you to more specialize care.
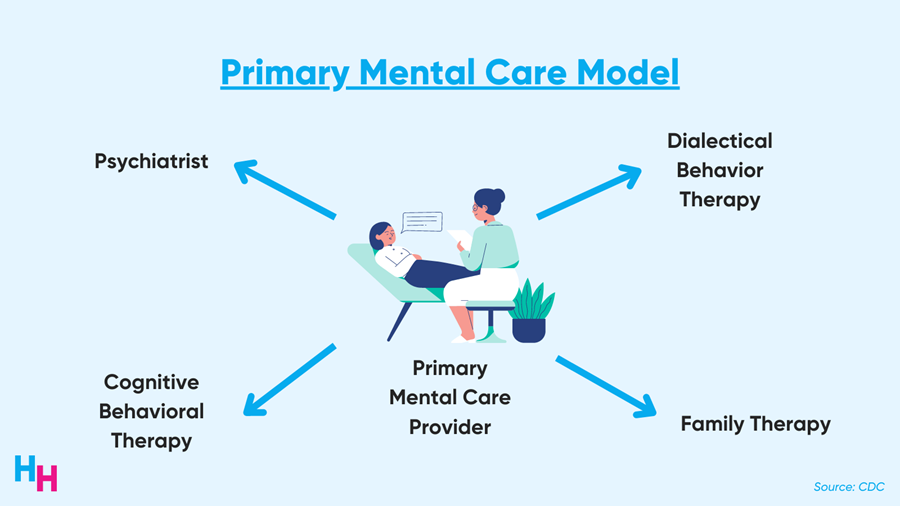
Say the PMCP recognizes signs of depression when speaking with you. Right then and there, they can engage you in psychotherapy. If psychotherapy doesn’t seem beneficial, the PMCP refers you to a psychiatrist who can prescribe appropriate medication. Or, say you develop panic disorder. Psychodynamic therapy may not be effective, so the PMCP refers you to a more specialized therapist that can deliver cognitive behavioral therapy.
The PMCP will also play a vital role for the developing child. Adverse childhood experiences (ACE) such as domestic violence, trauma (e.g., school shootings), parental divorce, abuse and neglect are strong predictors of future mental illness such as depression. I envision school counselors can quickly engage students in telehealth care with a PMCP as soon as an ACE is identified and provide appropriate therapy (or refer to more specialized mental care) to minimize the downstream effects of ACE.
Lastly, I envision the metaverse playing a significant role in therapy. For example, providers and patients will be able to enter the virtual reality of the metaverse and partake in treatment. Imagine what group therapy would look like? Patients from all over the community can don their VR set, enter the metaverse, see their peer patients and partake in therapy.
In summary, the future of psychotherapy mirrors the primary care models we currently have. The PMCP serves as the initial touchpoint in mental health care and can provide appropriate therapy and refer to more specialized therapy if needed.
You are what you eat, and drugs
We’re well aware of the influence the gut has on the brain and vice versa—what’s known as the gut-brain axis.
The gut-brain axis is the next frontier of gastroenterology and psychiatry. By 2032, I envision researchers will have elucidated much more information about the gut’s role on the brain, allowing for targeted therapies. For example, suppose researchers find a particular group of bacteria that may reduce depressive symptoms. In that case, perhaps patients can take a probiotic that adds said group of bacteria to the gut microflora.
I also envision robust nutrition tracking apps with behavioral logs. Every day, you track your food intake and behavioral metrics such as your mood, allowing the app to run some regression model correlating certain foods to specific moods.
Additionally, I imagine psilocybin will be a common therapy for depression. While recent phase 2 clinical trials found no significant difference in baseline depression scores between psilocybin and escitalopram, longer clinical trials may uncover significant differences, especially compared to other antidepressant medications such as bupropion. Similarly, I see ketamine—already FDA approved—being a more common treatment for depression, especially for treatment-resistant depression. Anecdotally and scientifically, ketamine works wonders for people with treatment-resistant depression.
Overall, I envision we’ll see startups prop up, focusing on therapeutics that target the gut-brain axis, and more widespread use of alternative depression therapy such as psilocybin and ketamine.
Closing Remarks
Once Henry Ford scaled the assembly line for automobile manufacturing, the industry blossomed. In just 100 years, we went from horses to autonomous electric vehicles.
In 2032, mental health tech will blossom with more robust tools to predict mental illness symptoms. The primary mental care model will expand access to mental health care and ensure patients are linked with the appropriate specialists. Funding for mental health research will pave the way for novel, widespread therapeutics. The following 10 years for mental health will be akin to what the automobile industry saw in 100 years. I cannot wait.
P.S.
If you have thoughts on what I predict, or have your own predictions, reply back to my Twitter thread (or to this email).

Thanks to those who already replied (Luke, Rik, Chris, Arpan, Tom, Jay, Erica and Marcella)! Share This Insight →

HOSPITALOGY THIS WEEK
Hospitalogy’s Week Ahead
This week’s Thursday deep dive will be Part 2 on health system mergers and where I think they’re headed. If you missed part 1, you can find it here.
Of course, Tuesday’s send will cover all of the relevant healthcare business news from the week. If you missed last week’s send, I talked about accountability in healthcare, specifically in reference to Cerebral and also Centura Health.
See ya Tues & Thurs as always, Hospitalogy fam. I hope you’re having a restful Memorial Day just like Jared.

MORE ON MENTAL HEALTH
- The Other Epidemic: What happens when one epidemic influences another?
- Digital Health’s Icarus: Did digital mental health startup Cerebral run an Adderall mill?
- The Great Resignation: The shortage of nurses, and the dooming exodus.
- Telehealth Balloons: Telehealth visits increased 63-fold among Medicare Part B beneficiaries.
- The 2021 Digital Health Explosion: 2021’s total digital health funding blows 2020’s funding out of the water.
- Akili Interactive: Video game therapeutics company Akili Interactive plans to go public via SPAC in a deal valued at $1B.

HUDDLE HITS
- My Meditation: washing the dishes is the way I meditate. Doing so grounds me in the present and prohibits me from looking at my phone.
- Where to find a therapist: I used headway.co to find my therapist. They find therapists that take your insurance so you can find the most affordable option!
- ✍️ Journal App: I journal every morning while I drink my coffee using the app Day One. I started using it last July and I love it.
- My favorite psych book: Man’s Search for Meaning by Viktor Frankl is one of my favorite books that is a must-read.

HEALTHCARE JOBS
Here are some jobs that I’m curating for the healthcare industry. Use this link to submit your role to be featured if you’re looking to hire.
Digital Health PR + Comms, HermesPR
Fast-growing boutique PR agency HermesPR is looking for someone to fill their PR and communications role. All entry levels! Candidates must have transferable experience in public relations or communications to be considered. Digital health or tech PR experience is required.
Medical Advisor, Otorhinolaryngologist, Cove
Cove is looking for experts in Otorhinolaryngology to be a Medical Advisor. Time requirements will vary on a monthly basis (typically 3-5 hours per month). Remote work.
Senior Growth Manager of Health Services, Hinge Health
Hinge is looking for someone who has Health Plan relationship management experience as a management consultant, vendor or other partner to lead their growth efforts. If you’re interested in health care and making a difference in people’s lives, and passionate about the intersection of technology and healthcare, then this is for you.View More →

FINAL THOUGHT
These past several weeks have been mentally exhausting and demoralizing, leaving many people—including me—feeling hopeless about the future of public health. I hope everyone finds time for themselves to recharge and reflect. You’re not alone. This is tough.
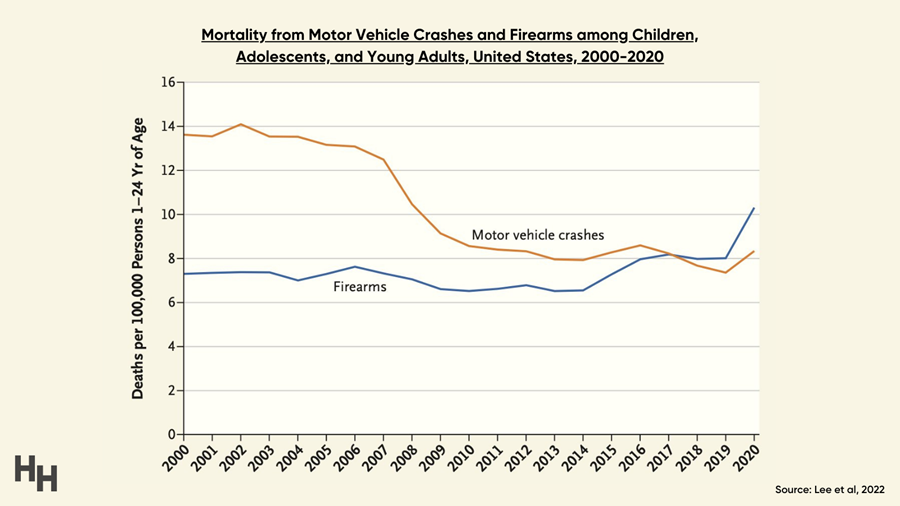
Mass shootings are a public health crisis unique to the United States. Compared to other high-income nations, the firearm homicide rate is 25x higher in the U.S. Even more upsetting: 97% of all children aged 0-4 years killed by guns worldwide were from the U.S. Firearms are now the leading cause of death among children and teens, surpassing motor vehicle accidents for the first time in history.
Once you’ve taken time for yourself, I encourage you to reach out to your state representatives and senators and plead for any sort of gun reform. At this point, any type of measure will help.

