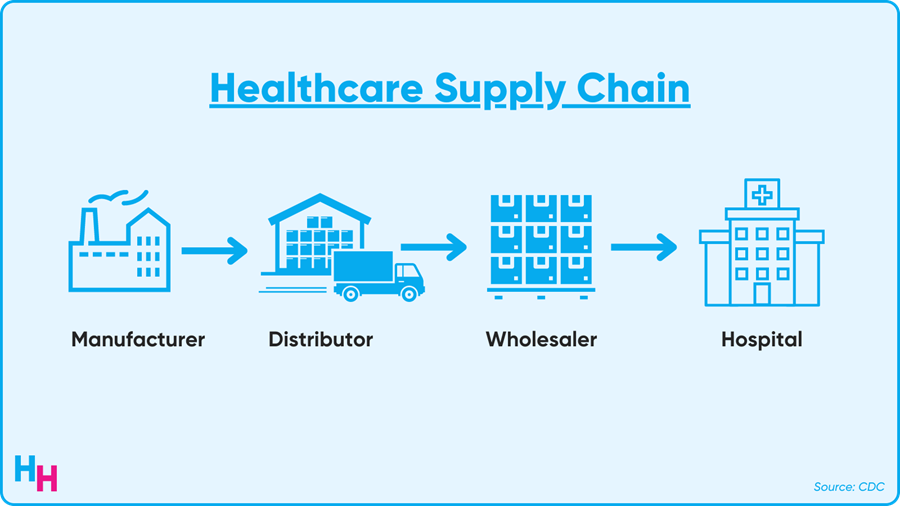
SUPPLY CHAIN
Healthcare Supply Chain Gone Haywire
Hospitals are grappling with yet another serious, pandemic-induced supply chain shortage. This time: intravenous contrast.
GE Healthcare’s production site in Shanghai shut down in April after the city went into another Covid-19 lockdown. Return to production has been slow. The company estimates the site is now operating at around 50% of its production capacity and expects to return to full capacity by the end of June.
GE Healthcare is one of the largest IV contrast manufacturers in the world and U.S. hospitals rely heavily on GE for their IV contrast for millions of patients annually.
This type of contrast is used for CT scans and fluoroscopy procedures—both of which are vital for diagnosing disease and intervening to prevent the progression of disease (e.g., cardiac catheterization). While we don’t have exact numbers yet showing the impact, anecdotally, it appears the U.S. is being hit hard by the shortage.
Thoughts
The pandemic revealed how frail the global healthcare supply chain is. We first saw this with masks and then with ventilators.
It seems history is repeating itself, albeit very quickly. Doctors, including radiologists, interventional cardiologists and neurologists who all rely on IV contrasts for diagnosing and intervening, are yet again faced with an all-to-familiar decision: who should or shouldn’t receive IV contrast for diagnostics or intervention. Dr. Christopher Hess from UCSF summed up nicely the implications of the contrast shortage:
If imaging services sneeze, then the whole health system gets the flu.
We’ll soon see just how bad the “flu” is once numbers start rolling in regarding the shortage’s impact on patients.
Nearly two years ago, Dr. Ezekiel J. Emanuel and his colleagues wrote an article about allocating scarce medical resources during Covid-19 fairly. They brought up four fundamental principles to consider when rationing, and I note how this may apply to the contrast shortage in italics:
- Maximize the benefits produced by scarce resources: Use contrast for emergent and urgent situations (cardiac catheterization, stroke patients, small bowel obstruction) to maximize lives saved. Routine procedures should be postponed.
- Treat people equally: You can’t really treat all patients equally in this case. Emergent and urgent patients should go first, since they’re at higher risk of morbidity and mortality. Patients after that could be randomly selected, assuming their prognoses would be similar.
- Promote and reward instrumental value: Not sure how this would work for contrast. But an example of vaccines: healthcare providers were first in line since being vaccinated would allow them to provide care for patients.
- Give priority to the worst off: Sickest go first, when doing so aligns with maximizing benefits (e.g., favorable prognosis).
While I hope this is the last supply chain shortage we have, I’m sure it won’t be. The pandemic has been broken record: cases increase, decrease, increase again; supply chain is fine, not fine, fine again; hospitals are financially stressed, not stressed, stressed again. It goes on and on. While Covid-19’s viral evolution may be out of our control, one thing that is in our control is the healthcare supply chains we rely on and how diverse we choose to make them.

HOSPITALOGY THIS WEEK
Hospitalogy’s Week Ahead
Everyone has been asking me, “Blake – WHERE are your thoughts on the Advocate-Atrium merger? What’s the strategy here? What are the broader implications for health systems?” Well…wait no longer. We’ll be diving deep this Thursday at 12pm ET on the history of health system M&A and how it’s evolving.
Of course, Tuesday’s send will cover all of the relevant healthcare business news from the week. I might even have my own take on the whole Cerebral situation. Guess you’ll have to see!
See ya Tues & Thurs, Hospitalogy fam.

DIGITAL MENTAL HEALTH
Join the thousands of healthcare professionals who read Hospitalogy
Subscribe to get expert analysis on healthcare M&A, strategy, finance, and markets.
No spam. Unsubscribe any time.
The Cerebral Shake-Up
Following the drama of mental health startup Cerebral has been like following a juicy show on Netflix—I can’t wait for the next episode to see what happens. In the last episode of Cerebral, I covered the new federal investigation into the company’s excessive prescribing of controlled ADHD medication. So what’s new for this week’s episode?
In This Week’s Episode
Amid the federal investigation, Cerebral decided to stop prescribing Adderall and benzodiazepines. Cerebral will no longer prescribe these meds to new patients and will stop prescribing them to established patients in October.
At the very same time, Cerebral’s board voted to remove CEO Kyle Robertson, citing a “lack of confidence in his leadership.” Dr. Muo is replacing him, but I’m not sure if this is the best swap—Dr. Muo seems to have played a substantial role in pushing for more ADHD diagnoses and Adderall prescriptions.
Thoughts
Profits over patients is a dangerous game. Look no further than Purdue Pharma and the opioid epidemic to see what profits over patients looks like. Unfortunately, I think Cerebral is yet another example of a healthcare company that became so fixated on making money, they forgot about the patients.
How did Cerebral get to this point, though?
At the beginning of the pandemic, the DEA added some flexibilities to the Ryan Haight Act. This act requires providers to have an in-person visit with a patient before prescribing a controlled substance such as Adderall or a benzodiazepine. Therefore, the DEA decided to temporarily scratch the “in-person visit” requirement for the duration of the public health emergency. Cerebral, who initially focused on depression treatment, saw the opportunity to expand into ADHD and sleep disorders, prescribing controlled medications like Adderall and benzodiazepines.
Cerebral is not alone. Done is another company targeting ADHD with Adderall, while Mindbloom is a company targeting psychedelic medicine with Ketamine (controlled drug). I predict these types of companies prescribing controlled substances will follow the same path as Cerebral—profits will become too attractive, clouding the aggressive push to diagnose and treat.
However, organizations like the American Psychology Association want the DEA to make the Ryan Haight Act flexibilities permanent. Should they be permanent? It’s tricky. On the one hand, these flexibilities increase access to mental health care. But, on the other hand, these flexibilities increase the potential for misuse.
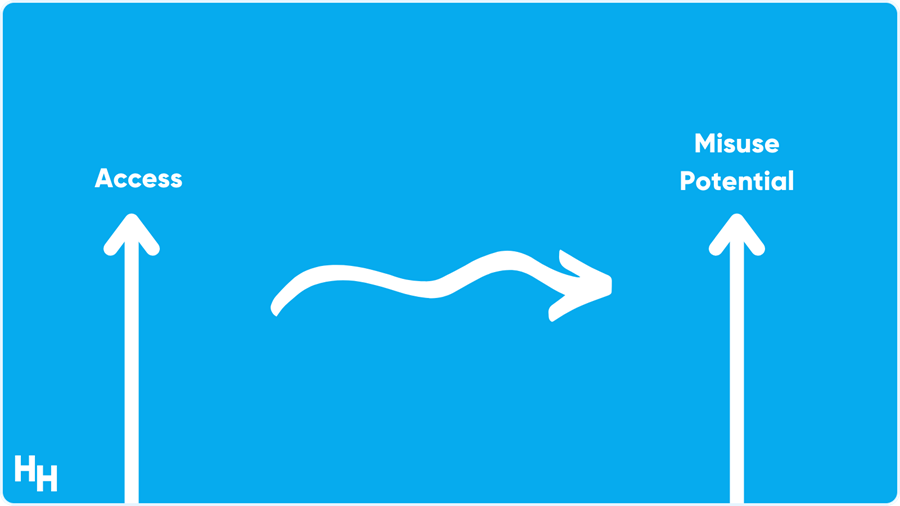
The government needs to find where the balance lies between access and misuse, and write rules accordingly to maximize access and minimize misuse.

DIGITAL HEALTH
Startups Addressing Care Gaps
Rock Health released a comprehensive report on startup innovation for underserved groups. Before summarizing their report, here’s a friendly reminder about U.S. healthcare compared to peer nations:
- We rank first in healthcare spending.
- We rank last in access to care.
- We rank last in equity.
- We rank last in outcomes.
- We rank last in administrative efficiency.
There’s a pressing need for startups to innovate around these areas of weakness to improve care for all groups of people. Rock Health’s report focuses on digital health innovation targeting groups that the healthcare system has marginalized, including rural communities, Medicaid beneficiaries, women of color and LGBTQ+ individuals.
Thoughts
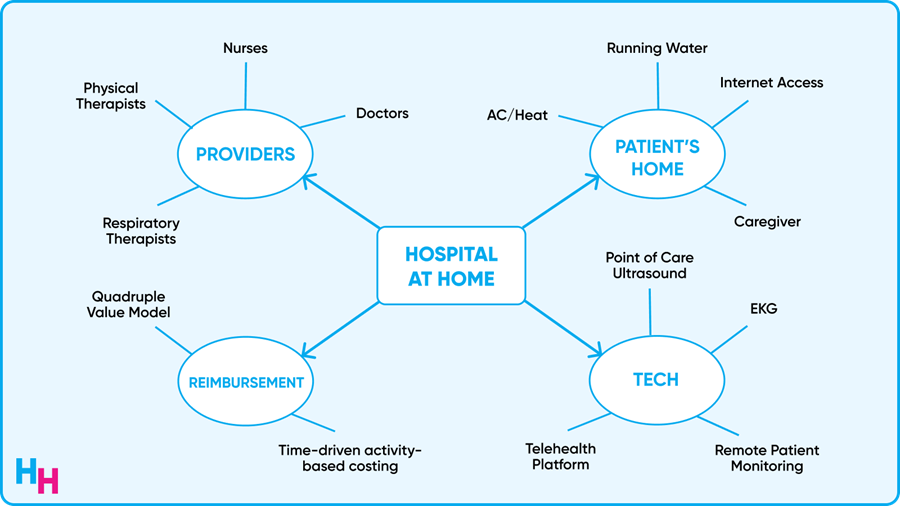
The report’s authors discuss over a dozen startups tackling the above areas, but here are my favorite startups they mentioned. Tackling rural communities is Origin Healthcare, which is bringing hospital-level care to patients’ homes. A couple of months ago I dove into Hospital at Home care models and why they’re becoming so popular. It wouldn’t surprise me if more companies like Origin Healthcare start sprouting up as the Hospital at Home trend continues.
Icario Health is a health action platform focused on Medicaid and Medicare populations. They use a multi-channel engagement approach to connect people to their health and are seeing rapid growth. I also love where their name comes from.
Mae is focused on an area of healthcare that no one (like the government) seems to be doing anything about: maternal health for Black women. Maternal mortality rates for Black women are three times higher than average, a disparity that has persisted for decades. Mae addresses this problem by providing pregnancy and postpartum support tailored to Black women’s needs. We need more startups like Mae.
Lastly, Violet’s educational platform helps providers grow and develop their LGBTQ+ cultural competency. They also have a benchmarking tool to evaluate team member’s progress. I like Violet’s mission. It adds structure to developing people’s cultural competency without having them attend sporadic, hour-long didactic sessions where people seldom pay attention or just forget everything they learned as soon as the session ends.

OUTSIDE THE HUDDLE
- Check out Blake Madden’s article on physician enablement care platform. These platforms offer physicians a higher level of autonomy without a lot of the headache that comes with owning a private practice.
- The good news: a study from Brigham and Women’s found a significant improvement in physician-reported patient safety after limiting first-year residents to 16 hours of consecutive work. The bad news: this policy was reversed in 2011. Resident work hours have always been an ongoing debate. At least the 80-hour work-week limit introduced in 2003 is still alive and well.
- By now, you’ve probably seen the words Monkeypox in your Twitter feed. The good news: we do know far more about Monkeypox than we did about Covid-19 at first. This isn’t the first time it’s spread in the US, and previous outbreaks were limited to dozens of cases. The bad news: there are cases not linked to travel from endemic countries (read: possible community spread), and we don’t know how large this outbreak will become.
- The growing number of unexplained hepatitis cases in pediatric patients has also gained worldwide attention. There have been 600 cases and 14 deaths worldwide. There have been 180 cases and six deaths in the U.S. alone, with 15 patients receiving liver transplants. Scientists are looking into an adenovirus strain as the culprit, but the cause is still largely unknown.
- Osmind, an EHR system geared towards mental health, secured a $40 million Series B. While Epic and Cerner’s systems dominate large health systems, Osmind may find a welcome home among smaller practices that provide mental health care.

